Showing posts with label alcohol treatment. Show all posts
Showing posts with label alcohol treatment. Show all posts
Tuesday, November 18, 2014
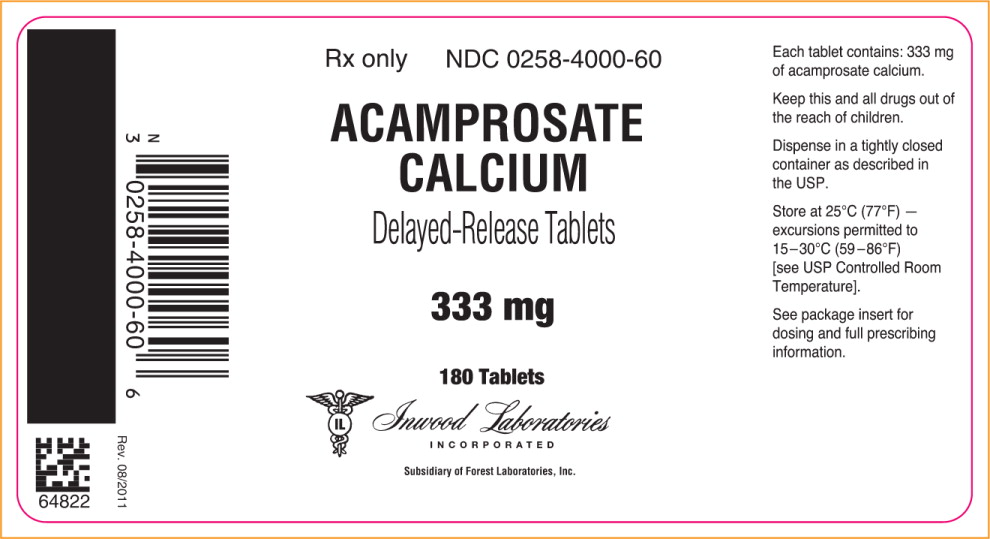
Another Look at Acamprosate
The most popular pharmaceutical treatment for alcoholism, explained.
(First published February 17, 2014)
“Occasionally,” reads the opening sentence of a commentary published online earlier this year in Neuropsychopharmacology, “a paper comes along that fundamentally challenges what we thought we knew about a drug mechanism.” The drug in question is acamprosate, and the mechanism of action under scrutiny is the drug’s ability to promote abstinence in alcoholics. The author of the unusual commentary is Markus Heilig, Chief of the Laboratory of Clinical and Translational Studies at the National Institute on Alcohol Abuse and Alcoholism (NIAAA).
Acamprosate, in use worldwide and currently the most widely prescribed medication for alcohol dependence in the U.S., may work by an entirely different mechanism than scientists have believed on the basis of hundreds of studies over decades. Rainer Spanagel of the Institute of Psychopharmacology at the University of Heidelberg, Germany, led a large research group in revisiting research that he and others had performed on acamprosate ten years earlier. In their article for Neuropsychopharmacology, Spanagel and coworkers concluded that a sodium salt version of acamprosate was totally ineffective in animal models of alcohol-preferring rats.
“Surprisingly,” they write, “calcium salts produce acamprosate-like effects in three animal models…. We conclude that N-acetylhomotaurinate is a biologically inactive molecule and that the effects of acamprosate described in more than 450 published original investigations and clinical trials and 1.5 million treated patients can possibly be attributed to calcium.”
At present, the Food and Drug Administration (FDA] has approved three drugs for alcoholism— Antabuse, naltrexone, plus acamprosate in 2004. In addition, there is considerable clinical evidence behind the use of four other drugs—topiramate, baclofen, ondansetron, and varenicline. Acamprosate as marketed is the calcium salt of N-acetyl-homotaurinate, a close relative of the amino acid taurine. It has also been found effective in European studies.
What did scientists think acamprosate was doing? Various lines of research had linked acamprosate to glutamate transmission. Changes in glutamate transmission have been directly implicated in active alcoholism. A decade ago, the Spanagel group had decided that acamprosate normalized overactive glutamate systems, and hypothesized that acamprosate was modulating GABA transmission. So it became known as a “functional glutamate antagonist.” But specific mechanisms have remained elusive ever since.
Now, as Heilig comments, “the reason it has been difficult to pin down the molecular site of acamprosate action may simply be because it does not exist. Instead, the authors propose that the activity attributed to acamprosate has all along reflected actions of the Ca++ it carries.” As the researcher paper explains it: “N-acetylhomotaurinate by itself is not an active psychotropic molecule…. We have to conclude that the proposed glutamate receptor interactions of acamprosate cannot sufficiently explain the anti-relapse action of this drug.” Further work shows that acamprosate doesn’t interact with glutamate binding sites at all. In other words, calcium appears to be the major active ingredient in acamprosate. Animal studies using calcium chloride or calcium gluconate reduced alcohol intake in animals at rates similar to those seen in acamprosate, the researchers claim.
Subsequently, the researchers revisited the earlier clinical studies, subjected them to secondary analysis, and concluded that “in acamprosate-treated patients positive outcomes are strongly correlated with plasma Ca++ levels. No such correlation exists in placebo-treated patients.” In addition, calcium salts delivered via different carrier drugs replicated the suppression of drinking in the earlier animal findings.
Where there cues pointing toward calcium? The researchers conclude that “calcium sensitivity of the synapse is important for alcohol tolerance development, calcium given intraventricularly significantly enhances alcohol intoxication in a dose-dependent manner,” and “activity of calcium-dependent ion channels modulate alcohol drinking.”
Interestingly, in the late 50s and early 60s, there was a brief period of interest in calcium therapy for the treatment of alcoholism. In 1964, the Journal of Psychology ran an article titled “Intensive Calcium Therapy as an Initial Approach to the Psychotherapeutic Relationship in the Rehabilitation of the Compulsive Drinker.” Now it appears possible that a daily dose of acamprosate is effective for some abstinent alcoholics because it raises calcium plasma levels. Calcium supplements may be in for a round of intensive clinical testing if these findings hold up.
The authors now call for “ambitious randomized controlled clinical trials,” to directly compare “other means of the Ca++ delivery as an approach to treat alcohol addiction. Data in support of a therapeutic role of calcium would open fascinating clinical possibilities.” Indeed it would.
Spanagel R., Vengeliene V., Jandeleit B., Fischer W.N., Grindstaff K., Zhang X., Gallop M.A., Krstew E.V., Lawrence A.J. & Kiefer F. (2013). Acamprosate Produces Its Anti-Relapse Effects Via Calcium, Neuropsychopharmacology, 39 (4) 783-791. DOI: 10.1038/npp.2013.264
Friday, June 27, 2014
Gone in June
Alcohol takes a friend.
What good does it do: You write about addiction, research it, think about it, formulate new ideas about it. You try to be of service.
What good does it do: One of your best friends ever, a talented writer you have talked to and argued with and smoked with and paddled with for more than two decades, lies dead this morning of alcohol-related liver failure at 62.
What good does it do: I couldn’t save him, couldn’t turn the head of that runaway horse, not through encouragement, shame, praise, incentive, disgust, indifference, furious anger. Not through any of that.
What good does it do: His doctor, with my help, presented a program of 30-day detox and Ativan for the rough parts. He ordered the pills, never picked them up at the pharmacy. He never went back to the doctor, claiming a lack of health insurance. He never quit. He tried, like so many deluded alcoholics, to cut back on his drinking. He kept the phone number for the local AA group in a desk drawer, but never called. When his girlfriend told him it was either her or the bottle, he picked the bottle.
What good does it do: We cajoled, we watched him, we tripped over bags of empties in the basement and he didn’t care. We couldn’t save him. I couldn’t save him. I know more about alcoholism than most addiction therapists, and I couldn’t save him. I saved myself, 25 years ago, but could not save him.
What good does it do: I don’t know how to treat alcoholism, and save alcoholics, and neither do you. And if anybody tells me today, the day of my friend’s death, that alcoholism is a lifestyle choice, I promise to throw a swift right cross and knock them out on the spot.
The only possible light on the horizon is continued scientific research aimed at better elucidating the mechanisms behind addiction. Without that, one idea is about as good as another.
Labels:
alcohol excess,
alcohol treatment,
alcoholism,
how to stop drinking,
rehab,
sober
Monday, February 17, 2014
Acamprosate For Alcohol: Why the Research Might Be Wrong
“Occasionally,” reads the opening sentence of a commentary published online last month in Neuropsychopharmacology, “a paper comes along that fundamentally challenges what we thought we knew about a drug mechanism.” The drug in question is acamprosate, and the mechanism of action under scrutiny is the drug’s ability to promote abstinence in alcoholics. The author of the unusual commentary is Markus Heilig, Chief of the Laboratory of Clinical and Translational Studies at the National Institute on Alcohol Abuse and Alcoholism (NIAAA).
Acamprosate, in use worldwide and currently the most widely prescribed medication for alcohol dependence in the U.S., may work by an entirely different mechanism than scientists have believed on the basis of hundreds of studies over decades. Rainer Spanagel of the Institute of Psychopharmacology at the University of Heidelberg, Germany, led a large research group in revisiting research that he and others had performed on acamprosate ten years earlier. In their article for Neuropsychopharmacology, Spanagel and coworkers concluded that a sodium salt version of acamprosate was totally ineffective in animal models of alcohol-preferring rats.
“Surprisingly,” they write, “calcium salts produce acamprosate-like effects in three animal models…. We conclude that N-acetylhomotaurinate is a biologically inactive molecule and that the effects of acamprosate described in more than 450 published original investigations and clinical trials and 1.5 million treated patients can possibly be attributed to calcium.”
At present, the Food and Drug Administration (FDA] has approved three drugs for alcoholism— Antabuse, naltrexone, plus acamprosate in 2004. In addition, there is considerable clinical evidence behind the use of four other drugs—topiramate, baclofen, ondansetron, and varenicline. Acamprosate as marketed is the calcium salt of N-acetyl-homotaurinate, a close relative of the amino acid taurine. It has also been found effective in European studies.
What did scientists think acamprosate was doing? Various lines of research had linked acamprosate to glutamate transmission. Changes in glutamate transmission have been directly implicated in active alcoholism. A decade ago, the Spanagel group had decided that acamprosate normalized overactive glutamate systems, and hypothesized that acamprosate was modulating GABA transmission. So it became known as a “functional glutamate antagonist.” But specific mechanisms have remained elusive ever since.
Now, as Heilig comments, “the reason it has been difficult to pin down the molecular site of acamprosate action may simply be because it does not exist. Instead, the authors propose that the activity attributed to acamprosate has all along reflected actions of the Ca++ it carries.” As the researcher paper explains it: “N-acetylhomotaurinate by itself is not an active psychotropic molecule…. We have to conclude that the proposed glutamate receptor interactions of acamprosate cannot sufficiently explain the anti-relapse action of this drug.” Further work shows that acamprosate doesn’t interact with glutamate binding sites at all. In other words, calcium appears to be the major active ingredient in acamprosate. Animal studies using calcium chloride or calcium gluconate reduced alcohol intake in animals at rates similar to those seen in acamprosate, the researchers claim.
Subsequently, the researchers revisited the earlier clinical studies, subjected them to secondary analysis, and concluded that “in acamprosate-treated patients positive outcomes are strongly correlated with plasma Ca++ levels. No such correlation exists in placebo-treated patients.” In addition, calcium salts delivered via different carrier drugs replicated the suppression of drinking in the earlier animal findings.
Where there cues pointing toward calcium? The researchers conclude that “calcium sensitivity of the synapse is important for alcohol tolerance development, calcium given intraventricularly significantly enhances alcohol intoxication in a dose-dependent manner,” and “activity of calcium-dependent ion channels modulate alcohol drinking.”
Interestingly, in the late 50s and early 60s, there was a brief period of interest in calcium therapy for the treatment of alcoholism. In 1964, the Journal of Psychology ran an article titled “Intensive Calcium Therapy as an Initial Approach to the Psychotherapeutic Relationship in the Rehabilitation of the Compulsive Drinker.” Now it appears possible that a daily dose of acamprosate is effective for some abstinent alcoholics because it raises calcium plasma levels. Calcium supplements may be in for a round of intensive clinical testing if these findings hold up.
The authors now call for “ambitious randomized controlled clinical trials,” to directly compare “other means of the Ca++ delivery as an approach to treat alcohol addiction. Data in support of a therapeutic role of calcium would open fascinating clinical possibilities.” Indeed it would.
Spanagel R., Vengeliene V., Jandeleit B., Fischer W.N., Grindstaff K., Zhang X., Gallop M.A., Krstew E.V., Lawrence A.J. & Kiefer F. (2013). Acamprosate Produces Its Anti-Relapse Effects Via Calcium, Neuropsychopharmacology, 39 (4) 783-791. DOI: 10.1038/npp.2013.264
Sunday, March 24, 2013
More Hard Facts About Addiction Treatment
“Yes, we take your insurance.”
Recent reportage, such as Anne Fletcher’s book, Inside Rehab, has documented the mediocre application of vague and questionable procedures in many of the nation’s addiction rehab centers. You would not think the addiction treatment industry had much polish left to lose, but now comes a devastating analysis of a treatment industry at “an ethics crossroads,” according to Alison Knopf’s 3-part series in Addiction Professional. Knopf deconstructs the problems inherent in America’s uniquely problematic for-profit treatment industry, and documents a variety of abuses. We are not talking about Medicaid, Medicare, or Block Grants here. Private sector dollars, Knopf reaffirms, do not “guarantee that the treatment is evidence-based, worth the money, and likely to produce a good outcome.” Even Hazelden, it turns out, is prepared to offer you “equine therapy,” otherwise known as horseback riding.
Knopf, who is editor of Alcoholism and Drug Abuse Weekly, was specifically looking at private programs, paid for by insurance companies or by patients themselves. Who is in charge of enforcing specific standards of business practice when it comes to private drug and alcohol rehabs? Does the federal government have some manner of regulatory control? According to a physician with the Substance Abuse and Mental Health Services Administration (SAMHSA), the feds rely on the states to do the regulating. And according to state officials, the states look to the federal agencies for regulatory guidance.
All too often, the states routinely license but do not effectively monitor treatment facilities, or give useful consumer advice. Florida state officials do not even know, with any certainty, exactly how many treatment centers are in operation statewide. And even if state monitoring programs were effective and aggressively applied, “just because something is legal doesn’t mean it’s ethical,” said the SAMHSA official.
“We see this as a pivotal time for the treatment field as we have come to know it,” said Gary Enos, editor of Addiction Professional, in an email exchange with Addiction Inbox. Enos said that “the Affordable Care Act (ACA) will move addiction treatment more into the mainstream of healthcare, and this will mean that treatment centers' referral and insurance practices will come under more scrutiny than ever before.”
Among the questionable practices documented by Knopf:
—Paying bounties and giving gifts to interventionists in return for client referrals.
Under Medicare, paying interventionists for referrals is banned. “In the private sector,” says a California treatment official, “it’s not illegal. But it is unethical.” According to treatment lobbyist Carol McDaid, “kickbacks happen all the time. Treatment centers that are doing this will do so at their own peril in the future,” she told Knopf.
—Giving assurances that treatment will be covered by insurance even though only a portion of the cost is likely to be covered.
Under the Affordable Care Act (ACA), says the SAMHSA official, “We are trying to position people to know more about their benefit package. And the industry has to be more straightforward about what the package will cover.” John Schwarzlose, CEO of the Betty Ford Center, told Knopf that “it’s very hard for ethical treatment providers to compete against insurance bait-and-switch,” when patients are told their insurance is good—but aren’t told that the coverage ends after 7 days, or that the daily maximum payout doesn’t meet the daily facility charges.
—Billing patients directly for proprietary nutrient supplements, brain scans, and other unproven treatment modalities.
“Equine therapy, Jacuzzi therapy, those are nice things, and maybe they help with the process of engagement,” said one therapist. “But people need to recognize that these ancillaries aren’t the essence of getting sober.”
—Engaging in dubious Internet marketing schemes.
You see them on the Internet: dozens and dozens of addiction and rehab referral sites. They list private services in various states, and look, on the surface, like legitimate information resources for people in need. As the owner of a blog about drugs and addiction, I hear from them constantly, asking me for links. “Family members and patients frequently have no way of knowing that a treatment program was really a call center they got to by Googling ‘rehab,’ writes Knopf, “and that the call center gets paid for referring patients to the actual treatment center. They don’t know that a program that promises to ‘work with’ health insurance knows full well the insurance will cover only a few days at the facility, and the rest will have to be paid out of pocket.” She points to a 2011 Wired magazine article, which said the Internet marketing cost of key words like “rehab” and “recovery” can be stratospheric. But “by spending that money—not necessarily providing good service—treatment provides can come out on top on searches. It’s the new marketing to the desperate.”
The group with the most to lose from revelations of this nature is the National Association of Addiction Treatment Providers (NAATP), the association representing both private and non-profit rehab programs. The Betty Ford Center has discontinued its membership in NAATP, a move that reflects the turmoil of the industry today. “It’s crazy that we have treatment centers inviting interventionists and other referents on a cruise, and then giving everyone an iPad,” Schwarzlose said.
As one man who lost his son to an overdose said: “I don’t get it. There’s the American Cancer Society, but I look for drugs and alcohol and I can’t find anything. There’s no National Association for Addictive Disease. How can this be?”
The investigative series will be featured in Addiction Professional’s March/April print issue. Enos believes that “influential treatment leaders are more interested than ever to see this debate aired more publically,” and says that the online publication of Knopf’s articles for the magazine has sparked “a great deal of discussion in treatment centers and on social media, including comments about other questionable practices that harm the field’s reputation.”
Tuesday, February 26, 2013
Addiction Rehab: Everything is Broken
Down the rabbit hole in search of effective treatment.
When I first began researching drugs and addiction years ago, a Seattle doctor told me something memorable. “It’s as if you had cancer,” she said, “and your doctor’s sole method of treatment consisted of putting you in a weekly self-help group.”
I’ve got nothing against weekly self-help groups, to be sure. But as Ivan Oransky, executive editor of Reuters Health and a blogger at Retraction Watch, told me as recently as least year, addiction treatment appeared to be “all selling and self-diagnosis. They’re selling you on the fact that you need to be treated.”
In his introduction to Inside Rehab by Anne M. Fletcher (pictured), treatment specialist and former deputy drug czar A. Thomas McLellan writes that the book is “filled with disturbing accounts of seriously addicted people getting very limited care at exhaustive costs and with uncertain results...”
A common notion about addiction treatment facilities, or rehabs, is they are commonly called, is that they are staffed by professional social workers, certified counselors, and family psychologists, as well as addiction specialists. However: “Of the twenty-one states that specify minimum educational requirements for program or clinical directors of rehabs, only eight require a master’s degree and just six require credentialing as an addiction counselor,” writes Fletcher. Neuroscience journalist Maia Szalavitz, who writes for Time Healthland and specializes in addiction and rehab, told Fletcher that “the addiction field has been about as effectively regulated as banking before the economic crisis in many states.” According to Tom McLellan, counselor and director turnover in addiction treatment programs is “higher than in fast-food restaurants.”
In the United States, where for-profit treatment is prevalent, money does not buy access to superior treatment. Fletcher, author of several self-help books on weight loss and alcoholism, doggedly documents what she learns from visiting treatment facilities and interviewing current and former staff and clients. One difficulty with a book of this kind, based primarily on first-hand accounts, is that the same treatment program can offer vastly contrasting experiences from one client to another. And Fletcher, no fan of the 12 Steps, wants AA and NA to account for themselves in a way those volunteer institutions were never designed to accomplish.
But let’s just say it: Addiction treatment in America is a disaster. Addicts get better despite the treatment industry as often as they get better because of it. How did it all go wrong? Part of the answer is that addiction, like depression, tuberculosis, and other chronic conditions, is a segregated illness, as McLellan explains in his introduction. Traditionally, chronic conditions like alcoholism “were not recognized as medical illnesses, and have only recently been taught in most medical schools and treated by physicians. They were seen as ‘lifestyle problems’ and care was typically provided by concerned, committed individuals or institutions not well connected to mainstream health care.”
For treatment of alcoholism and drug addiction, the work has historically fallen to addicts themselves, due to discrimination, segregation, and stigmatization. This prevailing condition is still seen today in many group treatment programs, which are often administered in large part by former addicts with little or no formal training, rather than medical or psychological professionals. Addiction, as the author’s husband wryly remarked, “is the only disease for which having it makes you an expert.”
Which brings up a central point: Where are all the M.D.s? Doctors aren’t helping, either, when they fail to screen for risky drinking or drug use, or when they automatically refer addicts rather than treating them.
If Christopher Kennedy Lawford’s new book, Recover to Live, is the pretty picture, then Fletcher’s Inside Rehab is the gritty picture, in which most addicts who recover don’t go to treatment, 28 days is not long enough to accomplish anything but detox, group counseling is not always the best way to treat addiction, the 12 Steps are not always essential to recovery, specialty drugs are often needed to treat drug addiction, and, perhaps the most troubling of all, most addiction programs do not offer state-of-the-art approaches to treatment that have been shown to be effective in scientific studies.
What clients get, for the most part, is “group, group, and more group,” Fletcher writes. And in many cases of residential or outpatient rehab, “the clients did most of the therapy.” The scientific evidence suggests that some addicts do better with an emphasis on individual counseling, rather than the constant reliance on group work that traditional rehabs have to offer. As one counselor put it: “If I made an appointment to see a therapist because I was depressed, would I be told I have to do a program with everyone else?”
Monthly residential treatment can easily cost $25,000 or more. But public, government funded rehab centers, which presumably have less incentive to treat clients like money, are frequently full. And since these programs run the bulk of prison-related treatment in this country, addicts often stand a better chance of getting into these less expensive programs if they commit a crime.
Even if you manage to get in, rehab rules all too often seem arbitrary and punitive: Recreational reading materials, musical instruments, cell phones, and computers are frequently not permitted. And there is a strong tendency to insist that use equals abuse in every circumstance. Rehab management—the business of what happens after formal treatment ends—is largely neglected in the treatment sphere.
Fletcher rails against the disease model, but mostly in response to how she believes this concept is presented by AA/NA. Like other critics, she dwells on the idea that the disease tag serves as a crutch and an excuse, rather than as an extremely empowering notion for many addicts. In fact, the disease model, as addiction scientists understand it, is seriously underrepresented in the treatment field. Too many mental health professionals continue to insist that “all you need to do is get to the bottom of the problem and the need to use substances to cope, will dissipate,” said an M.D. specializing in addiction. “However, there is absolutely no evidence that this approach works for people who are addicted to alcohol or drugs… The primary-secondary issue is moot and an artifact of the bifurcation of the treatment delivery system.”
A significant number of rehabs still oppose medication-assisted treatment, Fletcher makes clear. Hazelden made news recently for dropping its long-standing opposition to buprenorphrine as a maintenance drug for opiate addicts during treatment. Richard Saitz of Boston University’s School of Medicine says in the book that if addiction were viewed like other health problems, “patients addicted to opioids who are not offered the opportunity to be on maintenance medications would sue their providers and win.”
According to Dr. Mark Willenbring, former director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA): “No one wants to say, ‘Treatment as we’ve been doing it probably isn’t as effective as we thought, and we need more basic research to really come up with new tools. In the meantime let’s do what we can to help suffering people in the most cost effective way and strive to not harm them.’”
Wednesday, July 25, 2012
Broken Treatment: How the Addiction Industry is Failing its Clients
It’s not medical. It's not psychiatric. What is it?
1. Most clinicians who treat addicted patients are counselors, not physicians; thus they cannot prescribe medication and they generally don’t “believe” in the use of medication for addictive disorders.
2. Most patients have medical insurance that excludes or severely limits treatment of addictive disorders, so payment for service is not good. This situation may change in the near future with the advent of healthcare reform in the United States.
So writes Dr. Charles O’Brien of the University of Pennyslvania Perelman School of Medicine, in a recent article for The Dana Foundation’s website. In his article—“If Addictions Can Be Treated, Why Aren’t They?”—Dr. O’Brien asks a basic question: “Why are most patients not even given a trial of medication in most respected treatment programs?”
Even though pharmaceutical companies have throttled back on their interest in anti-craving drugs in recent years, there are, in fact, a few medications recognized by the FDA, primarily for use in the treatment of alcoholism. But they are not much in favor, and O’Brien believes he knows why:
The answer seems to be that there is a bias among treatment professionals, perhaps passed down from past generations when addictions were not understood to be a disease. Medically trained personnel are minimally involved in the addiction treatment system and most medical schools teach very little about addiction so most physicians are unaware of effective medications or how to use them.
What is on offer at most addiction treatment facilities is not actual rehabilitation, but rather short-term detoxification. And what we’ve learned from neuroscience is that taking away the drug is only stage one. The addiction remains, the reward and memory systems still operating erratically. We understand some of this circuitry better than at any time in history, but the concrete effects of these insights at the level of the community treatment clinic have been small to nonexistent. Money, of course, is part of it, since addiction has only recently, and sporadically, gotten the attention of funding agencies in the public health community.
Health journalist Maia Szalavitz, writing at Time Healthland concurs: “Unlike most known diseases, the treatment of addiction is not based on scientific evidence nor is it required to be provided by people with any medical education—let alone actual physicians—according to a new report.” The report in question, from Columbia University’s National Center on Addiction and Substance Abuse (CASA), notes that most people are shoehorned into a standardized approach built around the 12 Step model of Alcoholics Anonymous. “The dominance of the 12-step approach,” writes Szalavitz, “also leads to a widespread opposition to change based on medical evidence, particularly the use of medications like methadone or buprenorphine to treat opioid addictions—maintenance treatments that data have show to be most effective.”
Szalavitz also believes she knows why, and her thinking is similar to O’Brien’s. “Other medications that are known to treat alcohol and drug addiction, such as naltrexone, are also underutilized,” she writes, “while philosophical opposition to the medicalization of care slows uptake.”
There is a straightforward reason for considering the use of medication in the treatment of addiction: strong suggestions of recognizable genetic differences between those who respond to a given medication, and those who don’t. As O’Brien explains, a prospective study now in progress will be looking to see if alcoholics with a specific opioid receptor variant show a better outcome on naltrexone than those with the standard gene for that opioid receptor. And if they do, the FDA may allow a labeling change “stating that alcoholics with this genotype can be expected to have a superior response to naltrexone.”
But that won’t be happening tomorrow. In the meantime, we are stuck with the addiction treatment industry as it is. “The [CASA] report notes that only 10% of people with substance-use problems seek help for them,” Szalavitz concludes. “Given its findings about the shortcomings of the treatment system, that’s hardly surprising.”
Photo Credit: Creative Commons
Saturday, July 21, 2012
John Berryman and the Poetry of “Irresistible Descent”
“The penal colony’s prime scribe.”
“Will power is nothing. Morals is nothing. Lord, this is illness.”
—John Berryman, 1971
A year before he committed suicide by jumping off a Minneapolis bridge in 1972, Pulitzer Prize-winning poet John Berryman had been in alcohol rehab three times, and had published a rambling, curious, unfinished book about his treatment experiences. Recovery is a time capsule. If you think we have little to offer addicts by way of treatment these days, consider the picture in the 60s and 70s. In Recovery, treatment consists almost entirely of Freudian group analysis, and while there is regular talk of alcoholism as a disease, AA style, there is no evidence that it was actually dealt with in this way, after detoxification.
Best known for “Dream Songs,” Berryman taught at the University of Minnesota, and was known as a dedicated if irascible professor. Scientist Alan Severence, Berryman’s stand-in persona in the book, comes into rehab hard and recalcitrant, despite his previous failures: “Screw all these humorless bastards sitting around congratulating themselves on being sober, what’s so wonderful about being sober? Great Christ, most of the world is sober, and look at it!” And he is suffering from “the even deeper delusion that my science and art depended on my drinking, or at least were connected with it, could not be attacked directly. Too far down.”
Berryman was a difficult man, and knew it. He quotes F. Scott Fitzgerald: “When drunk, I make them pay and pay and pay and pay.”
Alcoholics, writes Berryman, are “rigid, childish, intolerant, programmatic. They have to live furtive lives. Your only chance is to come out in the open.” Berryman catches the flavor of group interaction after too many hours, too much frustration, and too much craving. One inpatient lashes out: “You’re lying when you say you do not do anything about your anger. You get bombed. It is called medicating the feelings, pal. Every inappropriate drinker does it. Cause and effect. Visible to a child. Not visible to you.”
Berryman was a shrewd observer, a singular writer, and, after all, a poet. He is extraordinary on the subject of alcoholic dissociation: “I found myself wondering whether I would turn off right towards the University and the bus home or whether I would just continue right on to the Circle and up right one block to the main bar I use there, and have a few. Wondering. My whole fate depending on pure chance…. as if one were not even one’s own actor but only a spectator.”
Berryman puts it all together in a horrific capsule description of the “irresistible descent, for the person incomprehensibly determined.”
Relief drinking occasional then constant, increase in alcohol tolerance, first blackouts, surreptitious drinking, growing dependence, urgency of FIRST drinks, guilt spreading, unable to bear discussion of the problem, blackout crescendo, failure of ability to stop along with others (the evening really begins after you leave the party)… grandiose and aggressive behavior, remorse without respite, controls fail, resolutions fail, decline of other interests, avoidance of wife and friends and colleagues, work troubles, irrational resentments, inability to eat, erosion of the ordinary will, tremor and sweating… injuries, moral deterioration, impaired and delusional thinking, low bars and witless cronies….
Berryman had no illusions about his failed attempt to hide behind the mask of a social drinker: “It seems to be loss of control. Unpredictability. That’s all. A social drinker knows when he can stop. Also, in a general way, his life-style does not arrange itself around the chemical, as ours does. For instance, he does not go on the wagon…”
In the end, he was "pleading the universal case of hope for abnormal drinkers, for all despairing and deluded sufferers fighting for their sanity in a world not much less insane itself and similarly half-bent on self-destruction…”
As the head nurse in the facility tells the group: “You are all suffering from the lack of self-confidence… often so powerful that it leads to consideration of suicide, a plan which if adopted will leave you really invulnerable, quite safe at last.”
And as Saul Bellow wrote in the introduction to Recovery: “At last there was no more. Reinforcements failed to arrive. Forces were not joined. The cycle of resolution, reform and relapse had become a bad joke which could not continue.” Berryman agreed. Toward the end, he wrote: “I certainly don’t think I’ll last much longer.”
“There’s hope until you’re dead,” a woman tells him during his final stay in rehab. Sadly, that hope ended a few months later.
Photo posted by Tom Sutpen for the series: Poets are both clean and warm
Sunday, September 20, 2009
Kudzu for Alcoholism?

Common vine extract may inhibit drinking.
Score one for traditional Chinese folk medicine. A compound called daidzin, found in kudzu vine, acts like the anti-drinking medication Antabuse. Daidzin interferes with the metabolization of alcohol and causes the well-known flushing and sick feeling associated with Antabuse.
However, Dr. Ivan Diamond of the University of California in San Francisco and Dr. Ting-Kai Li of Duke University Medical Center maintain that a synthetic derivative of the active ingredient in kudzu vine also helps diminish the desire to drink in alcoholic rats. It does so, they believe, by preventing alcohol-induced increases in dopamine in the brain’s pleasure center. This additional finding about daidzin may help prevent relapse in recovering alcoholics by diminishing cravings—something Antabuse does not do.
The study will be published in the November issue of Alcoholism: Clinical and Experimental Research.
Currently, the commonly prescribed medications for alcoholism include disulfiram (Antabuse), naltrexone (Revia and Vivitrol), acamprosate (Campral), topiramate (Topamax), and baclofen (Lioresal).
Harvard researchers Wing Ming Keung and Bert Vallee first discovered the effects of kudzu on drinking. A 2005 paper in Alcoholism: Clinical and Experimental Research, authored by Scott E. Lukas, et. al., reported the results of testing a kudzu extract on a clinical population of “heavy” drinkers. The result: “Kudzu treatment resulted in significant reduction in the number of beers consumed... and a decrease in the volume of each sip.” The earlier researchers, however, did not report any significant effect on the urge to drink.
In their recent research, Diamond and Li believe they have found a synthetic version of daidzin, CVT-1-216, that does effect the desire to drink. According to Diamond, the study found that the drug “prevents the usual increase in drinking (binge drinking) that occurs after five days of abstinence....”
“Extracts of various parts of the kudzu vine have been used in many Chinese herbal medicine formulas and are said to be helpful in treating a variety of maladies,” said Dr. Li, who was formerly the director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA). “The findings show promise that CVT-10216 might be better tolerated than Antabuse,” he added.
Dr. Diamond called alcoholism “a medical disorder, not just a problem of will power. Physicians treat medical disorders in order to prevent harm, while not necessarily curing the disease being treated—for example, drug treatment of hypertension, stains for high cholesterol, insulin for diabetes—and the same will become true for treating alcoholism.”
Diamond also agrees that synthetic kudzu extract may prove superior to Antabuse in other ways. “Most believe that disulfiram (Antabuse) would not be approved today as a new drug for alcoholism because of its many toxicities.”
Photo Credit: www.skrewtips.com
Thursday, January 1, 2009
Recovery in 2009

Some resolutions for the New Year.
The SoberRecovery site has put up a forum entitled: "Anybody up for New Year Resolutions?" You can read the thread at the link above. There are old ones, new ones, and in-between ones.
From the practical...
“i will buy an accordion folder (if santa doesn't bring me one)--and i will organize my recipes”.
To the whimsical...
“I want a *real* accordion."
From the personal...
“To practice the golden rule even in heavy traffic.”
To the profound...
“My New Year's Resolution is to embrace life--to fully come out of the tiny, insular, self-absorbed world that drinking kept me in for so long and live to my full potential!
And organize my garage!”
Happy New Year to All.
Dirk Hanson
Site editor, Addiction Inbox
Graphic Credit: Vox Sacramento
Saturday, August 16, 2008
Nothing Beats Booze

Annual survey ranks alcohol as #1 problem.
Drugs may make headlines, but alcohol is the elephant sitting in the corner of the room, according to Community Anti-Drug Coalitions of America (CADCA), a non-profit organization that conducts an annual survey of community anti-drug service groups. CADCA, sponsored in part by the U.S. Department of Health and Human Services, found that 68 percent of community anti-drug coalitions ranked alcohol as “the number one problem facing their community.”
The group said that marijuana was in second place, listed by 60 percent of communities as one of the major problems in their areas. Tobacco was a close third.
“It’s no surprise that our members are seeing big problems with youth alcohol use in their communities,” said Arthur T. Dean, CADCA chairman and CEO. 700 community anti-drug coalitions took part in the 2007 survey. Community anti-drug coalitions rely on strategies including media outreach, advertisements, educational events and community forums.
Asked to name the major partners helping them tackle community drug problems, 88 percent of survey respondents listed “law enforcement.” That was slightly ahead of the number of respondents listing “parents” (86 percent).
While the results cannot be considered a surprise, it is disheartening to discover that an earlier CADCA survey found that the “alcohol stigma” is alive and well: 63 percent of Americans still believe alcoholism is a moral weakness. Only 34 percent of respondents labelled it a disease. The earlier survey also reported that two out of every five Americans reported that they have encouraged a loved one to seek help for an alcohol problem.
Moreover, a group of Britain’s most prominent drug researchers published a report in the Lancet last year calling for the U.K. to scrap its current drug classification scheme in favor of one that “more honestly reflects the harm caused by alcohol and tobacco,” according to an article in the U.K Guardian by science correspondent James Randerson.
The study team “asked 29 consultant psychiatrists who specialise in addiction to rate [20 drugs of abuse] in nine categories. Three of these related to physical harm, three to the likelihood of addiction and three to social harms such as healthcare costs,” writes Randerson. In the final rankings, heroin and cocaine were ranked as the most dangerous. Alcohol placed 5th, well ahead of marijuana (11th), LSD (14th), and Ecstasy (18th).
Predictably, howls of outrage and shock were heard from dozens of U.K. politicians and anti-drug crusaders after the report was published.
Photo Credit: LiveJournal
Monday, July 21, 2008
Drugs for Alcoholism

Different meds for different drinkers
Although there are still only three drugs officially approved by the FDA for the treatment of alcoholism, the research picture is beginning to change. In an article by Greg Miller published in the 11 April 2008 edition of Science, alcoholism researcher Stephanie O'Malley of Yale University said: "We have effective treatments, but they don't help everyone. There's lots of room for improvement."
The medications legally available by prescription for alcoholism are: disulfiram (Antabuse), naltrexone (Revia and Vivitrol), and acamprosate (Campral), the latest FDA-approved entry. A fourth entry, topiramate (Topamax), is currently only approved by the Food and Drug Administration (FDA) for use against seizures and migraine. The controversial practice of “off-label” prescribing—using a drug for indications that are not formally approved by the FDA—has become so common that Johnson & Johnson said it had no plans to seek formal approval for the use of Topamax as a medicine for addiction. (See my post,"Topamax for Alcoholism: A Closer Look").
Addiction experts are beginning to focus on which treatment drugs work best for different types of alcoholics. Two recent discoveries might help clarify the picture. Psychopharmacologist Charles O'Brien at the University of Pennsylvania reported that alcoholics with a specific variation, or allele, of a prominent opioid receptor gene were more likely to respond positively to treatment with naltrexone. Other work reported in the February 2008 Archives of General Psychiatry came to the same conclusion.
The second research insight builds on a lifetime of work by Robert Cloninger at Washington University in St. Louis. Cloninger discovered that alcoholics come in two basic flavors--Type 1 and Type 2. Type 1, the more common form, develops gradually, later in life, and does not necessarily require structured intervention. Type 1 alcoholics do not always experience the dramatic declines in health and personal circumstances so characteristic of acute alcoholism. These are the people often found straddling the line between alcoholic and problem drinker. In contrast, so-called Type 2 alcoholics are in serious trouble starting with their first taste of liquor during adolescence. Their condition worsens with horrifying speed. They frequently have a family history of violent and antisocial behavior, and they often end up in prison. They are rarely able to hold down normal jobs or sustain workable marriages for long. Type 2s, also known as “familial” or “violent” alcoholics, are likely to have had an alcoholic parent.
Type 1 drinkers, who only get in trouble gradually, are also known as "anxious" drinkers, and research suggests that they may respond better to medicines that alleviate alcohol-related anxiety, such as Lilly's new suppressor of stress hormones, known as LY686017. (See my post, "Drug That Blocks Stress Receptor May Curb Alcohol Craving "). Researchers at the National Institute of Alcohol Abuse and Alcoholism (NIAAA), working with colleagues at Lilly Research Laboratories and University College in London, announced the discovery of a drug that diminished anxiety-related drug cravings by blocking the so-called NK1 receptor (NK1R). The drug “suppressed spontaneous alcohol cravings, improved overall well-being, blunted cravings induced by a challenge procedure, and attenuated concomitant cortisol responses.”
The NIAAA researchers are making effective use of recent findings about the role played by corticotrophin-releasing hormone (CRH) in the addictive process. CRH is crucial to the neural signaling pathway in areas of the brain involved in both drug reward and stress. As it happens, NK1R sites are densely concentrated in limbic structures of the mid-brain, such as the amygdala, or so-called “fear center.”
Researchers are understandably excited about these developing insights. Psychopharmacologist Rainer Spanagel of Germany's Central Institute of Mental Health in Mannheim called such research "a milestone in pharmacogenetics." In Greg Miller's Science article, Willenbring of NIAAA predicted that the field is poised for a "Prozac moment," marked by the discovery of "a medication that's perceived as effective, that's well-marketed by a pharmaceutical company, and that people receive in a primary-care setting or general-psychiatry setting."
In "Days of Wine and Roses, " the 1960s film about alcoholism, Jack Lemmon played a character who embodied Type 2 characteristics--early trouble with alcohol, extreme behavioral dysregulation, poor long-term planning, and a hollow leg. His wife, played by Lee Remick, demonstrates the slower, more measured descent from problem drinking into clinical alcoholism that characterizes Type 1 alcoholics. Research now suggests that Lee Remick might do better on LY686017, while Jack Lemmon's character would be a promising candidate for treatment with naltrexone.
Photo credit: About Alcohol Information
Thursday, May 29, 2008
Annals of Addiction: Richard Lewis

From The Harder They Fall
"It's hard to know exactly when I became an alcoholic. What I do know is that growing up I felt misunderstood, not appreciated, and needing validation. I didn't feel I was getting it from important people in my life. They had their problems, their own concerns. I felt sort of invisible....
"Drinking made me feel not as miserable. It was a great Band-Aid. It progressed, but it didn't stop me in my career. I've done well, and I was an alcoholic at the height of my career, when I really hit. When alcohol really got me by the throat, I quit stand-up comedy. Acting was easier. Easier to stay sober most of the time, do my work, and know I'm off for three days.....
"There were tip-offs, even way early. I remember getting some sort of sexually transmitted disease that was going to last for a week. I had to take certain antibiotics, and I remember the doctor very nonchalantly saying, 'Oh, by the way, you can't drink for five days.' I was going to New York to appear on the Letterman show, and all I thought about was, 'Oh my God, there I am in first class, five-and-a-half hours in an airplane, without booze. There I am in New York with my friends and no booze. I can't even have a couple of glasses of wine in my hotel room to relax before the show.' That's all I thought about. I wasn't thinking of my career. I wasn't thinking about anything but 'I can't believe I can't drink.' It was horrifying. And that was thirteen years before I bottomed.
"I was hallucinating. I was emaciated. Holed up doing coke for six nights.... I was ashamed to waste my life, given all the blessings I had. That I would throw away my life needlessly. To have a disease that I could stop giving myself, if I surrendered, finally.....
"One reason I love being sober is that I thought about this guy I saw who slipped last week, who I spoke to this morning.... I wouldn't have been able to do that if I was drinking. I couldn't have helped this guy.... If I'm going to leave any kind of legacy, making people laugh is fine, but to help somebody get the darkness from out of their eyes and to turn their life around, it's the most important aspect of my life."
Excerpted from:
The Harder They Fall, by Gary Stromberg and Jane Merrill. Center City, MN: Hazelden.
Photo Credit: Pearlies of Wisdom
Labels:
alcohol treatment,
alcoholism,
celebrity rehab,
Richard Lewis
Wednesday, May 28, 2008
Annals of Addiction: Grace Slick

From The Harder They Fall
"There's a whole bunch of alcoholics on both sides of my family, but they function in the sense that everybody kept their jobs. There were no divorces, except for my grandmother, but she's not an alcoholic. She was just a wild child like I was. Our alcoholics all kept their jobs and stayed married....
"The Airplane became famous as the original psychedelic band, but personally, I was more of a drinker. Anything that was around and easy I took--marijuana was very easy to score, but alcohol was my drug of choice. That's the genetic deal going on, where I'm an addict in the sense that anything I like I'm all over. Like flies on shit! And sometimes that works out fine. Right now I'm a painter. That's how I make my living and pay the mortgage....
"In 1970, when I became pregnant with China, I wasn't conscious of addiction. My life was all just sex, drugs and rock and roll. But I'm not a moron, so I knew that what you put into your face goes into your body, and part of your body is what's living in there--the child....
"Life is now fine. My daughter is sober. China came in a couple of weeks after me. Into the same rehab. My sponsor was amused. She had never seen a mother-daughter combination in the same rehab....
"I always felt very close to the story of Alice in Wonderland for a real good reason. If you remember what happened to her, she came from a very straight-laced Episcopalian Republican background, and at some point between twelve and twenty-four--mine at about eighteen or so--you go down the rabbit hole."
Excerpted from:
The Harder They Fall, by Gary Stromberg and Jane Merrill. Center City, MN: Hazelden.
Photo Credit: Donna E. Natale Planas/Miami Herald
Monday, May 26, 2008
Annals of Addiction: Malcolm McDowell

From The Harder They Fall
"My father was an alcoholic, so I never really drank much. I kept away from it, but I didn't realize that cocaine was really the same thing. Alcohol eventually started getting a little out of control, but in the form of 'fine wine.' That was my excuse....
"So I didn't consider wine a problem, but cocaine was a problem, and that got out of hand quite fast. It had a very bad effect on my marriage. The lies and deceit and everything that goes with addiction. I went from snorting it occasionally to now smoking it, doing freebase. Doing as much as I could. Finish a batch at four in the morning. Driving around the San Fernando Valley looking for some more of it. Driving while completely stoned, of course. How I was never in an accident, I just don't know....
"The using ended because I went down to the Betty Ford Center.... I didn't thank God at the time time, however. I felt I'd lost a great friend or mistress, that I'd lost the one thing that I could totally trust--all that bullshit! It wasn't until I started to work on myself at Betty Ford, which is a wonderful place as is any place that gets you sober....And, of course, it's hard work, recovery. Less and less hard as the years have gone by, but you know, the way we live our lives is all recovery in one sense or another. We go through a shattering experience like that, and everything we do in life from then on is in a way influenced by what we've been through."
Excerpted from:
The Harder They Fall, by Gary Stromberg and Jane Merrill. Center City, MN: Hazelden.
Photo Credit: MTV News
Saturday, May 3, 2008
Ten Things to Know about Addiction

From "Rethinking Substance Abuse."
In the closing chapter of their 2006 book, "Rethinking Substance Abuse,” editors William R. Miller and Kathleen M. Carroll attempt to sum up what has been learned about the science of addiction. Their useful contribution, entitled Drawing the Science Together, offers "Ten Principles" that are designed to synthesize the welter of recent scientific research on addiction and help make sense of what we know.
In vastly truncated form, they are as follows:
1. Drug Use is Chosen Behavior
At least in the beginning, people choose to take drugs, as one of the behavioral options available to them.
2. Drug Problems Emerge Gradually
"Dependence emerges over time, as the person's life becomes increasingly centered on drug use," the authors write. "The diagnostic criteria for classifying people with 'drug abuse' and 'drug dependence' represent arbitrary cut points along a gradual continuum" (p.296).
3. Once Well Established, Drug Problems Tend to Become Self-Perpetuating
Once regular drug use has caused dysregulation of limbic reward systems, addictive behaviors "take on a life of their own," and become "surprisingly resistant to ordinary forces of persuasion, religion, punishment, and self-control. It can be challenging to destabilize such a self-organizing system" (p.296).
4. Motivation is Central to Prevention and Intervention
Miller and Carroll write: "Taking action also predicts change. Better outcomes follow from attending more sessions or staying longer in treatment, going to more 12-step meetings, adhering to treatment advice, or faithfully taking one's medication. It appears that actively doing something toward change may be more important than the particular actions that are taken" (p.297).
5. Drug Use Responds to Reinforcement
"Drug use tends to be associated with a foreshortening of time perspective, so that longer term delayed rewards are discounted in value.... People who more steeply discount delayed rewards are at higher risk for drug use and problems; moreover, drug use exacerbates discounting. Some effective medications reduce the reward value of drug use, which can enhance the appeal of alternative reinforcers" (p. 298).
6. Drug Problems Do Not Occur in Isolation, but as Part of Behavior Clusters
In young people, drug abuse often co-exists with mood disorders, behavioral problems at school or the job, and anti-social behaviors. As Miller and Carroll remind us, the same is true of adults. Family violence, health problems, unemployment, and child neglect are frequently associated with cases of active addiction.
7. There Are Identifiable and Modifiable Risk and Protective Factors for Problem Drug Use
"It is clear that heredity contributes to risk for alcohol problems, and evidence is mounting for genetic predispositions for or against other drug use" (p.299).
8. Drug Problems Occur within a Family Context
In addition to the evidence pointing to a direct genetic mode of transmission, parental drug use is also a risk factor. Anything that delays an addiction-prone young person from first use of alcohol or other drugs decreases the risk of long-term addiction.
9. Drug Problems Are Affected by a Larger Social Context
"Social isolation is both a promoter and a consequence of the progression of drug dependence, and social bonding with nonusers can be an antidote" (p.301).
10. Relationship Matters
In formal treatment settings, effectively matching counselor to client is crucial. Confrontational counselor styles are generally "countertherapeutic."
Graphics Credit: University of Utah, Genetic Science Learning Center
Friday, March 14, 2008
Drug That Blocks Stress Receptor May Curb Alcohol Craving

Anxiety, drugs, and the brain’s “fear center.”
A brain receptor for a neurotransmitter involved in stress and anxiety has become a primary target in the scientific war on alcoholism—the only kind of drug war that really matters.
Researchers at the National Institute of Alcohol Abuse and Alcoholism (NIAAA), working with colleagues at Lilly Research Laboratories and University College in London, announced that a drug that blocks the so-called NK1 receptor (NK1R) reduced alcohol cravings in a study of 25 detoxified alcoholic inpatients. The drug “suppressed spontaneous alcohol cravings, improved overall well-being, blunted cravings induced by a challenge procedure, and attenuated concomitant cortisol responses.”
The study, published in the current issue of Science magazine, (look here for abstract) demonstrates that investigators continue to work toward more effective anti-craving drugs from a variety of angles. The NIAAA researchers are making effective use of recent findings about the role played by corticotropin-releasing hormone (CRH) in the addictive process. CRH is crucial to the neural signaling pathway in areas of the brain involved in both drug reward and stress.
Another neurotransmitter of this type is substance P, together with its preferred receptor, NK1R. As it happens, NK1R sites are densely concentrated in limbic structures of the mid-brain, such as the amygdala, or so-called “fear center.” The experimental drug, known as LY686017, blocks NK1R receptors, shutting off substance P, which in turn diminishes anxiety-related drug cravings.
Other researchers had previously demonstrated that deletion of NK1R sites eliminated opiate use in animal models. It has also been known for some time that alcohol and the opiates share certain common chemical pathways in the brain. And in humans, at least one earlier study showed decreased stress and anxiety reactions in human subjects taking a drug that blocked the Neurokinin 1 receptors.
The authors of the study suggest that “blockade of NK1Rs might modulate stress- and reward-related processes of importance for excessive alcohol use and relapse.”
According to NIAAA director Dr. Ting-Kai Li, “These findings advance our understanding of the link between stress and alcohol dependence and raise the prospect of a new class of medications for treating alcoholism.”
The early finding will require more research. “To our knowledge,” the authors conclude, “no data are presently available to address this hypothesis.”
graphic credit: http://www.ibiblio.org/rcip/ptsdmemory.html
Friday, February 15, 2008
Soros Funds Addiction Initiative

Urges insurance companies to close “treatment gap.”
In a move designed to jump-start a reluctant insurance industry, philanthropist George Soros is pushing an addiction initiative aimed at the estimated 20 million Americans who cannot afford treatment for substance abuse.
Through his New York-based Open Society Institute (OSI), Soros will award $10 million in grants to study “obstacles associated with addiction treatment.” Victor Capoccia, who previously ran community-based drug and alcohol treatment programs for the Boston Department of Health and Hospitals, will serve as director of OSI’s Initiative to Close the Addiction Treatment Gap. Capoccia also directed the addiction prevention effort at the Robert Wood Johnson Foundation.
Any future system of universal health care should provide coverage of addiction as a medical condition, the group believes. “We’re going to look at the role of the public sector, and ask government to pay for people who lack insurance, not as a replacement for what other insurance should be paying for,” Dr. Capoccia told Alcoholism and Drug Abuse Weekly. “We don’t want public funds subsidizing what should be an insurance responsibility for this health issue.”
Among the issues the initiative will explore are the expansion of Medicaid to cover science-based addiction treatment, an emphasis on early intervention and aftercare, and increased funding of treatment programs from a variety of sources. Backers of the Soros initiative maintain that drug addiction is a health issue that should fall within the general financing of existing health care delivery systems.
“People with a health condition ought to have that condition treated,” Capoccia told the Baltimore Sun in an article by Michael Hill. “They should not be jailed or shunned or put aside until their condition is so acute that they are a hopeless case.”
Capoccia described addiction as a chronic disease like diabetes and hypertension. “Using that chronic disease framework,” he told the Sun, “you realize that this is a condition you have to learn to manage. It is not a case of finding a cure, that it’s here today and gone tomorrow. It is a process of mitigation, of reducing the harmful effects, reducing the behaviors associated with those harmful effects.”
Capoccia pointed to Baltimore and San Francisco as communities where local governments have focused effectively on addiction treatment, and have “helped build a sense of collaboration…between health departments and law enforcement in really positive ways."
Addiction, said Capoccia, “has all these impacts, yet we decide to provide the resources so only one in 10 gets help. It’s laughable.”
Grants will be for $600,000. Specific information about the funding program is available at http://www.soros.org/initiatives/treatmentgap/focus_areas/guidelines
Photo Credit: The Washington Note
Subscribe to:
Posts (Atom)