Showing posts with label rehab. Show all posts
Showing posts with label rehab. Show all posts
Sunday, November 13, 2016
Take It Easy
Labels:
12 Steps,
AA,
addiction,
addiction recovery,
alcoholics anonymous,
recovery,
rehab
Monday, June 20, 2016
Addiction Treatment Industry at the Crossroads
How unethical treatment shills hunt down patients.
Check this account at Huffington Post by Ryan Grim: "Addiction Treatment Industry Worried Lax Ethics Could Spell Its Doom."
Eye-opening.
Check this account at Huffington Post by Ryan Grim: "Addiction Treatment Industry Worried Lax Ethics Could Spell Its Doom."
Eye-opening.
Labels:
addiction treatment,
inside rehab,
rehab
Wednesday, September 17, 2014
Why Will Power Fails
How to strengthen your self-control.
(First published August 12, 2013)
Reason in man obscured, or not obeyed,
Immediately inordinate desires,
And upstart passions, catch the government
From reason; and to servitude reduce
Man, till then free.
—John Milton, Paradise Lost
What is will power? Is it the same as delayed gratification? Why is will power “far from bulletproof,” as researchers put it in a recent article for Neuron? Why is willpower “less successful during ‘hot’ emotional states”? And why do people “ration their access to ‘vices’ like cigarettes and junk foods by purchasing them in smaller quantities,” despite the fact that it’s cheaper to buy in bulk?
Everyone, from children to grandparents, can be lured by the pull of immediate gratification, at the expense of large—but delayed—rewards. By means of a process known as temporal discounting, the subjective value of a reward declines as the delay to its receipt increases. Rational Man, Economic Man, shouldn’t behave in a manner clearly contrary to his or her own best interest. However, as Crockett et. al. point out in a recent paper in Neuron “struggles with self-control pervade daily life and characterize an array of dysfunctional behaviors, including addiction, overeating, overspending, and procrastination.”
Previous research has focused primarily on “the effortful inhibition of impulses” known as will power. Crockett and coworkers wanted to investigate another means by which people resist temptations. This alternative self-control strategy is called precommitment, “in which people anticipate self-control failures and prospectively restrict their access to temptations.” Good examples of this approach include avoiding the purchase of unhealthy foods so that they don’t constitute a short-term temptation at home, and putting money in financial accounts featuring steep penalties for early withdrawal. These strategies are commonplace, and that’s because people generally understand that will power is far from foolproof against short-term temptation. People adopt strategies, like precommitment, precisely because they are anticipating the possibility of a failure of self-control. We talk a good game about will power and self-control in addiction treatment, but the truth is, nobody really trusts it—and for good reason. The person who still trusts will power has not been sufficiently tempted.
The researchers were looking for the neural mechanisms that underlie precommitment, so that they could compare them with brain scans of people exercising simple self-control in the face of short-term temptation.
After behavioral and fMRI testing, the investigators used preselected erotic imagery rated by subjects as either less desirable ( smaller-sooner reward, or SS), or more highly desirable ( larger-later reward, or LL). The protocol is complicated, and the analysis of brain scans is inherently controversial. But previous studies have shown heightened activity in three brain areas when subjects are engaged in “effortful inhibition of impulses.” These are the dorsolateral prefrontal cortex (DLPFC), the inferior frontal gyrus (IFG), and the posterior parietal cortex (PPC). But when presented with opportunities to precommit by making a binding choice that eliminated short-term temptation, activity increased in a brain region known as the lateral frontopolar cortex (LFPC). Study participants who scored high on impulsivity tests were inclined to precommit to the binding choice.
In that sense, impulsivity can be defined as the abrupt breakdown of will power. Activity in the LFPC has been associated with value-based decision-making and counterfactual thinking. LFPC activity barely rose above zero when subjects actively resisted a short-term temptation using will power. Subjects who chose the option to precommit, who were sensitive to the opportunity to make binding choices about the picture they most wanted to see, showed significant activity in the LFPC. “Participants were less likely to receive large delayed reward when they had to actively resist smaller-sooner reward, compared to when they could precommit to choosing the larger reward before being exposed to temptation.”
Here is how it looks to Molly Crockett and her fellow authors of the Neuron article:
Precommitment is adaptive when willpower failures are expected…. One computationally plausible neural mechanism is a hierarchical model of self-control in which an anatomically distinct network monitors the integrity of will-power processes and implements precommitment decisions by controlling activity in those same regions. The lateral frontopolar cortex (LFPC) is a strong candidate for serving this role.
None of the three brain regions implicated in the act of will power were active when opportunities to precommit were presented. Precommitment, the authors conclude, “may involve recognizing, based on past experience, that future self-control failures are likely if temptations are present. Previous studies of the LFPC suggest that this region specifically plays a role in comparing alternative courses of action with potentially different expected values.” Precommitment, then, may arise as an alternative strategy; a byproduct of learning and memory related to experiences “about one’s own self-control abilities.”
There are plenty of caveats for this study: A small number of participants, the use of pictorial temptations, and the short time span for precommitment decisions, compared to real-world scenarios where delays to greater rewards can take weeks or months. But clearly something in us often knows that, in the immortal words of Carrie Fisher, “instant gratification takes too long.” For this unlucky subset, precommitment may be a vitally important cognitive strategy. “Humans may be woefully vulnerable to self-control failures,” the authors conclude, “but thankfully, we are sometimes sufficiently far-sighted to circumvent our inevitable shortcomings.” We learn—some of us—not to put ourselves in the path of temptation so readily.
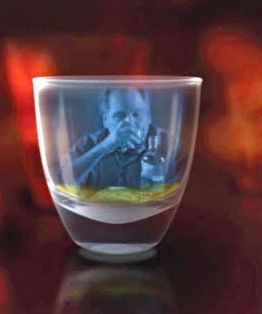
Photo Credit: http://cassandralathamjones.wordpress.com/
Labels:
AA,
addiction,
higher power,
rehab,
relapse,
treatment,
will power
Sunday, July 20, 2014
Drugs and Disease: A Look Forward
First published 2/18/2014.
Former National Institute on Drug Abuse (NIDA) director Alan Leshner has been vilified by many for referring to addiction as a chronic, relapsing “brain disease.” What often goes unmentioned is Leshner’s far more interesting characterization of addiction as the “quintessential biobehavioral disorder.”
Multifactorial illnesses present special challenges to our way of thinking about disease. Addiction and other biopsychosocial disorders often show symptoms at odds with disease, as people generally understand it. For patients and medical professionals alike, questions about the disease aspect of addiction tie into larger fears about the medicalization of human behavior.
These confusions are mostly understandable. Everybody knows what cancer is—a disease of the cells. Schizophrenia? Some kind of brain illness. But addiction? Addiction strikes many people as too much a part of the world, impacted too strongly by environment, culture, behavior, psychology, to qualify. But many diseases have these additional components. In the end, the meaning of addiction matters less than the physiological facts of addiction.
One of the attractions of medical models of addiction is that there is such an extensive set of data supporting that alignment. Specifically, as set down in a famous paper by National Institute of Drug Abuse director Nora Volkow and co-author Joanna Fowler: “Understanding the changes in the brain which occur in the transition from normal to addictive behavior has major implications in public health…. We postulate that intermittent dopaminergic activation of reward circuits secondary to drug self-administration leads to dysfunction of the orbitofrontal cortex via the striato-thalamo-orbitofrontal circuit.” This cascade of events is often referred to as the “hijacking” of the brain by addictive drugs, but nothing is really being hijacked. Rather, the abusive use of drugs changes the brain, and that should come as no surprise, since almost everything we do in the world has the potential of changing the brain in some way. “Why are we so surprised that when you take a poison a thousand times, it makes some changes in your head?” said the former director of a chemical dependency treatment program at the University of Minnesota. “It makes sense that [addictive drugs] change things.”
Critics like Fernando Vidal object to a perceived shift from “having a brain” to “being a brain.” He is saying that he cannot see the point of “privileging” the brain as a locus for the study of human behavior. In “Addiction and the Brain-Disease Fallacy,” which appeared in Frontiers in Psychiatry, Sally Satel and Scott Lillienfeld write that “the brain disease model obscures the dimension of choice in addiction, the capacity to respond to incentives, and also the essential fact people use drugs for reasons (as consistent with a self-medication hypothesis).”
An excellent example of the excesses of the anti-brain discussions is an article by Rachel Hammer of Mayo Clinic and colleagues, in the American Journal of Bioethics-Neuroscience. “Many believed that a disease diagnosis diminishes moral judgment while reinforcing the imperative that the sick persons take responsibility for their condition and seek treatment.” But only a few paragraphs later, the authors admit: “Scholars have theorized that addiction-as-disease finds favor among recovering addicts because it provides a narrative that allows the person simultaneously to own and yet disown deviant acts while addicted.” Furthermore: “Addiction reframed as a pathology of the weak-brained (or weak-gened) bears just as must potential for wielding stigma and creating marginalized populations." But again, the risk of this potentially damaging new form of stigma “was not a view held by the majority of our addicted participants…”
And so on. The anti-disease model authors seem not to care that addicted individuals are often immensely helped by, and hugely grateful for, disease conceptions of their disorder, even though Hammer is willing to admit that the disease conception has “benefits for addicts’ internal climates.” In fact, it often helps addicts establish a healthier internal mental climate, in which they can more reasonably contemplate treatment. Historian David Courtwright, writing in BioSocieties, says that the most obvious reason for this conundrum is that “the brain disease model has so far failed to yield much practical therapeutic value.” The disease paradigm has not greatly increased the amount of “actionable etiology” available to medical and public health practitioners. “Clinicians have acquired some drugs, such as Wellbutrin and Chantix for smokers, Campral for alcoholics or buprenorphine for heroin addicts, but no magic bullets.” Physicians and health workers are “stuck in therapeutic limbo,” Courtwright believes.
“If the brain disease model ever yields a pharmacotherapy that curbs craving, or a vaccine that blocks drug euphoria, as some researchers hope,” Courtwright says, “we should expect the rapid medicalization of the field. Under those dramatically cost-effective circumstances, politicians and police would be more willing to surrender authority to physicians.” The drug-abuse field is characterized by, “at best, incomplete and contested medicalization.” That certainly seems to be true. If we are still contesting whether the brain has anything essential to do with addiction, then yes, almost everything about the field remains “incomplete and contested.”
Sociologists Nikolas Rose and Joelle M. Abi-Rached, in their book Neuro, take the field of sociology to task for its “often unarticulated conception of human beings as sense making creatures, shaped by webs of signification that are culturally and historically variable and embedded in social institutions that owe nothing substantial to biology.”
And for those worried about problems with addicts in the legal system, specifically, over issues of free will, genetic determinism, criminal culpability, and the “diseasing” of everything, Rose and Abi-Rached bring good news: “Probabilistic arguments, to the effect that persons of type A, or with condition B, are in general more likely to commit act X, or fail to commit act Y, hold little or no sway in the process of determining guilt.” And this seems unlikely to change in the likely future, despite the growing numbers of books and magazine articles saying that it will.
Opponents of the disease model of addiction and other mental disorders are shocked, absolutely shocked, at the proliferation of “neuro” this and “neuro” that, particularly in the fields of advertising and self-improvement, where neurotrainers and neuroenhancing potions are the talk of the moment. Sociologists claim to see some new and sinister configuration of personhood, where a journalist might just see a pile of cheesy advertising and a bunch of fast-talking science hucksters maneuvering for another shot at the main chance. When has selling snake oil ever been out of fashion?
For harm reductionists, addiction is sometimes viewed as a learning disorder. This semantic construction seems to hold out the possibility of learning to drink or use drugs moderately after using them addictively. The fact that some non-alcoholics drink too much and ought to cut back, just as some recreational drug users need to ease up, is certainly a public health issue—but one that is distinct in almost every way from the issue of biochemical addiction. By concentrating on the fuzziest part of the spectrum, where problem drinking merges into alcoholism, we’ve introduced fuzzy thinking with regard to at least some of the existing addiction research base. And that doesn’t help anybody find common ground.
Graphics Credit: http://www.docslide.com/disease-model/
Labels:
12 step,
AA,
alcohol as disease,
disease model,
drug addiction,
drug treatment,
rehab
Friday, June 27, 2014
Gone in June
Alcohol takes a friend.
What good does it do: You write about addiction, research it, think about it, formulate new ideas about it. You try to be of service.
What good does it do: One of your best friends ever, a talented writer you have talked to and argued with and smoked with and paddled with for more than two decades, lies dead this morning of alcohol-related liver failure at 62.
What good does it do: I couldn’t save him, couldn’t turn the head of that runaway horse, not through encouragement, shame, praise, incentive, disgust, indifference, furious anger. Not through any of that.
What good does it do: His doctor, with my help, presented a program of 30-day detox and Ativan for the rough parts. He ordered the pills, never picked them up at the pharmacy. He never went back to the doctor, claiming a lack of health insurance. He never quit. He tried, like so many deluded alcoholics, to cut back on his drinking. He kept the phone number for the local AA group in a desk drawer, but never called. When his girlfriend told him it was either her or the bottle, he picked the bottle.
What good does it do: We cajoled, we watched him, we tripped over bags of empties in the basement and he didn’t care. We couldn’t save him. I couldn’t save him. I know more about alcoholism than most addiction therapists, and I couldn’t save him. I saved myself, 25 years ago, but could not save him.
What good does it do: I don’t know how to treat alcoholism, and save alcoholics, and neither do you. And if anybody tells me today, the day of my friend’s death, that alcoholism is a lifestyle choice, I promise to throw a swift right cross and knock them out on the spot.
The only possible light on the horizon is continued scientific research aimed at better elucidating the mechanisms behind addiction. Without that, one idea is about as good as another.
Labels:
alcohol excess,
alcohol treatment,
alcoholism,
how to stop drinking,
rehab,
sober
Tuesday, January 28, 2014
Going Deep: Surgery For Addiction?
Controversial DBS technique shows early promise for Parkinson’s, Tourette’s.
Bielefeld, Germany—
The third in an irregular series of posts
about a recent conference, Neuroplasticity in Substance Addiction and Recovery: From Genes to
Culture and Back Again. The conference, held at the Center for
Interdisciplinary Research (ZiF) at Bielefeld University, drew
neuroscientists, historians, psychologists, philosophers, and even a freelance
science journalist or two, coming in from Germany, the U.S., The Netherlands,
the UK, Finland, France, Italy, Australia, and elsewhere. The organizing idea
was to focus on how changes in the brain impact addiction and recovery, and
what that says about the interaction of genes and culture. The conference
co-organizers were Jason Clark and Saskia Nagel of the Institute of Cognitive Science at the University of Osnabrück,
Germany. Part One is here.
Part Two is here.
All addictive drugs increase the production of dopamine in the nucleus accumbens, as do other highly pleasurable activities. Part of the medial forebrain bundle (MFB), which mediates punishment and reward, the nucleus accumbens is the ultimate target for the dopamine released by the ingestion of cocaine, for example. The nucleus accumbens is a very old and evolutionarily well-preserved structure in the brain. If you remove large slices of the nucleus accumbens, or knock it out entirely, animals no longer want addictive drugs.
This is essentially the same pathway that regulates our food and water-seeking behavior. By directly or indirectly influencing the molecules of pleasure, alcohol and other drugs trigger key neurochemical events that are central to our feelings of both reward and disappointment. In this sense, the reward pathway is a route to both pleasure and pain. Studies of the nucleus accumbens have demonstrated abnormal firing rates in scanned addicts who were deep into episodes of craving. The craving for a reward denied causes dopamine levels in the nucleus accumbens to crash dramatically, as they do when users go off drugs.
During his presentation in Bielefeld, “Stimulating the Addictive Brain,” Dr. Jens Kuhn of the University Hospital of Cologne walked the audience through an explanation of one of the most controversial addiction treatment options of all, known as deep brain stimulation. For those unfamiliar with DBS, this surgical procedure uses implanted brain electrodes and a subdermal set of wires connected to a small power source to directly stimulate a designated area of the brain via electric current. Deep brain stimulation (DBS) is becoming an established treatment option for some movement disorders, in particular Parkinson’s disease. It is also being investigated for obsessive–compulsive disorder, major depression, and Tourette’s syndrome.
Kuhn and his researchers, the first German group to investigate deep brain stimulation beginning in 2002, started by investigating Tourette’s and OCD. But soon, Kuhn said, it became clear that “valid animal studies show significant induced improvement in cocaine, morphine and alcohol addiction behavior following DBS of the nucleus accumbens…. the few patients who underwent DBS surgery for addiction remained abstinent or had a major reduction of relapses.”
This is essentially the same pathway that regulates our food and water-seeking behavior. By directly or indirectly influencing the molecules of pleasure, alcohol and other drugs trigger key neurochemical events that are central to our feelings of both reward and disappointment. In this sense, the reward pathway is a route to both pleasure and pain. Studies of the nucleus accumbens have demonstrated abnormal firing rates in scanned addicts who were deep into episodes of craving. The craving for a reward denied causes dopamine levels in the nucleus accumbens to crash dramatically, as they do when users go off drugs.
During his presentation in Bielefeld, “Stimulating the Addictive Brain,” Dr. Jens Kuhn of the University Hospital of Cologne walked the audience through an explanation of one of the most controversial addiction treatment options of all, known as deep brain stimulation. For those unfamiliar with DBS, this surgical procedure uses implanted brain electrodes and a subdermal set of wires connected to a small power source to directly stimulate a designated area of the brain via electric current. Deep brain stimulation (DBS) is becoming an established treatment option for some movement disorders, in particular Parkinson’s disease. It is also being investigated for obsessive–compulsive disorder, major depression, and Tourette’s syndrome.
Kuhn and his researchers, the first German group to investigate deep brain stimulation beginning in 2002, started by investigating Tourette’s and OCD. But soon, Kuhn said, it became clear that “valid animal studies show significant induced improvement in cocaine, morphine and alcohol addiction behavior following DBS of the nucleus accumbens…. the few patients who underwent DBS surgery for addiction remained abstinent or had a major reduction of relapses.”
Carrie Wade and others at the Scripps Research Institute and Aix-Marseille University in France electrically stimulated the subthalamic nucleus and got addicted rats to take less heroin and become less motivated for the task of bar pressing to receive the drug. Earlier work had demonstrated a similar effect in rats’ motivation for cocaine use. “This research takes a non-drug therapy that is already approved for human use and demonstrates that it may be an option for treating heroin abuse,” Wade said in a prepared statement.
Dr. Kuhn told the audience that DBS is a “focused neuromodulation procedure to enrich electrical activity” applied to certain brain regions and requiring only “minimally invasive” surgery. In the case of DBS surgery for addiction, which Dr. Kuhn has performed in clinical settings, the target is the nucleus accumbens, which Kuhn called “the key player in the so-called limbic reward loop.”
The problem is that these investigations, while positive in many cases, are small and scattered thus far, and do not represent a systematic investigation of the procedure by the field of neuroscience at large. Not yet, anyway. And maybe not ever. There are very few published studies on human addicts, Kuhn said, “but luckily, the ethical implications of DBS are being more and more discussed.”
Unfortunately, as Kuhn pointed out, “neurosurgical interventions in psychiatric patients raise ethical considerations not only based on the disreputable experiences of the era of psychosurgery.” But that’s a good starting point. The procedure, despite one’s best efforts, conjures up images of “psychosurgery”—prefrontal lobotomies, or early electroconvulsive shock therapy (ECT). It doesn’t help that the likeliest mechanism of action that explains DBS is that high frequency stimulation causes functional lesions at the specific brain sites. From almost every angle, it seems ham-handed and crude—until you see some videos of results, like this one of a Tourette’s patient: Video
Kuhn acknowledged that a number of medical professional believe DBS is a poor choice for addiction, and its use “is premature due to expenses, possible risks and the assumed poor scientific rationale of the method in this field.” In a letter to the journal Addiction, Adrian Carter and Wayne Hall of the University of Queensland, Australia, noted that some of the positive reports come from China, where scientists have experimented with ablation of portions of the nucleus accumbens and other brain areas. And it seems to work. So, one cure for addiction has been discovered already—but surgically removing chunks of the midbrain isn’t likely to catch on, except as a seminar topic for medical ethicists. Carter and Hall call the evidence base for the safety and efficacy of DBS in addiction “weak,” and argue that “the addition of an expensive neurosurgical treatment that costs of the order of $50,000 will worsen this situation by utilizing scare health resources to treat a very small number of patients with the income to pay for it.”
In a history of “stereotactic lesions” as a treatment for movement disorders, researchers at The George Washington University School of Medicine and Health Sciences reviewed efforts to expand the use of DBS to include specific psychiatric disorders like depression and obsessive-compulsive disorders. Writing in the Journal of Neurosurgery in 2010, they concluded that “addiction and schizophrenia showed the least improvement from surgery. Therefore, pursuing the treatment of these disorders with DBS using the targets in these studies may be ineffective.”
The Neurotech Business Report recently documented that St. Jude Medical, a manufacturer of surgical devices, has shut down its clinical trial of DBS for depression (h/t Vaughan Bell). The company’s website said “The BROADEN (BROdmann Area 25 DEep brain Neuromodulation) Study” has been closed and is no longer enrolling participants. The article suggests that “the complexity of specifying the precise brain circuits involved with major depression” may have been the reason for halting the trial.
Known risks associated with deep brain stimulation placement include: dizziness, infection, loss of balance, and speech or vision problems. In addition, the devices, wires and leads that make up the system, which are all implanted in the brain or under the skin, can break or fail in various ways. DBS can also alter glucose metabolism and food intake in lab rats. Altogether, there are few case reports, and the mechanism of action remains essentially uncharacterized. In the case of addiction, this is one treatment that does not seem ready for prime time. It would be premature to move DBS beyond the clinical trial stage in humans without additional data.
Wednesday, January 22, 2014
Drug Craving, or How to Be Your Own Worst Enemy
Plus the disease model, warts and all.
Bielefeld, Germany—
The second in an irregular series of posts about a recent conference, Neuroplasticity in Substance Addiction and Recovery: From Genes to Culture and Back Again. The conference, held at the Center for Interdisciplinary Research (ZiF) at Bielefeld University, drew neuroscientists, historians, psychologists, philosophers, and even a freelance science journalist or two, coming in from Germany, the U.S., The Netherlands, the UK, Finland, France, Italy, Australia, and elsewhere. The organizing idea was to focus on how changes in the brain impact addiction and recovery, and what that says about the interaction of genes and culture. The conference co-organizers were Jason Clark and Saskia Nagel of the Institute of Cognitive Science at the University of Osnabrück, Germany. Part One is here.
Marc Lewis, a developmental neuroscientist who is currently professor of human development and applied psychology at Radboud University in The Netherlands, and who spent five days discussing addiction with the Dalai Lama and a small group of scientists, scholars, and addiction specialists in Dharamsala, India, last year, was a late but welcome addition to the speaker list at the conference.
Author of Memoirs of an Addicted Brain, and a self-confessed “drug addict turned neuroscientist,” Dr. Lewis always brings a thought-provoking dual perspective to his work on addiction. (See my review of his book here.) He also blogs here.
In Bielefeld, Dr. Lewis offered up a wide-ranging view of what addiction is and is not, linking neuroscience, psychology, and Buddhism in the process.
Craving is “the one condition all addicts agree is their worst enemy,” Lewis said. “This is one place where science and subjectivity have to come together. Scientists need to focus on this, because addicts are completely unanimous about it. This is the enemy. It’s not physical withdrawal symptoms, it’s not relief. It is craving.”
Buddhism teaches that “craving is the fundamental engine of personality development,” Lewis said. “It’s what keeps us going around and around.” But if you don’t much like the notion of the wheel of reincarnation, Lewis suggested, then you can contemplate “the cyclical nature of how we repeat patterns in life that lead to suffering.”
“Craving is such an unpleasant state, that after a while, you end up doing it, you get the drugs. I did opiates, and I would spend hours and hours trying to sit on my hands, trying to watch something on TV, trying to go for a walk, and finally, there’s this thing that keeps rising in the background, and it doesn’t go away. It was a constantly growing tension, an anxiety and discomfort, that came from very deep down. You spend most of your energy trying to hold this thing at bay, and according to the ego depletion literature, you can’t do that for very long. These cognitive control centers just give up. They are limited resources.”
Craving is not a steady state. It grows. “Neuroscience helps us understanding why craving is so nasty.” Enter “delay discounting,” a term from behavioral economics used by several speakers during the conference. Delay discounting is the proposition that the perceived value of something rises steeply as the reward gets closer in time. A variation of this idea is seen in the classic marshmallow test for children: One marshmallow now, or two if you wait until later?
“Craving traps you in delay discounting,” said Lewis. “Immediate reward is worth more than imagined future happiness. The job of dopamine in the striatum is to increase the attractiveness or value of one goal, and to reduce the attractiveness and value of all the other goals. This is a brain that is well designed for addiction. You get tons of dopamine rising up in anticipation of reward. So you’re really stuck in the immediate. At which point you’ve effectively lost contact with the rest of your life. In the narrative of who you are, you can’t even include next week, or the next morning.”
Nonetheless, Lewis finds serious problems with the standard disease model of addiction, as championed by NIDA’s Nora Volkow and other in the NIH, however brain-based he may be. As a developmental neuroscientist, Lewis is predisposed to viewing the brain as a locus of change by definition. “The disease model uses brain change as a foundational premise. But brains change with development, anyway. And in fact, brains are designed to change.”
Any proper model of addiction, he insisted, has to correspond with what we know about brain change. “But it also has to correspond with addicts’ experiences. I was a drug addict from about age 25 to 30. I was in really bad shape. And now I talk with a lot of drug addicts, and one of the things that I keep hearing is that scientists and clinicians don’t really know what they’re doing—they don’t know where to go with it. They know that addiction is really nasty, but they don’t know what it’s like, unless they’ve been there.”
Lewis offered a view of addiction that shifts the semantic focus from disease to development. The drug is not the culprit. By reconceptualizing addiction as a developmental disorder, he suggested, we can move the debate forward into the world, where the action is:
Addiction results from accelerated learning, the acquisition of thought patterns that rapidly self-perpetuate because of the brain’s tendency to become sensitized to highly attractive rewards. This is a developmental process, accelerated by a neurochemical feedback loop that is particular to strong attractions. Like other developmental outcomes, addiction isn’t easy to reverse, because it’s based on synaptic restructuring. Like other developmental outcomes, it arises from neural plasticity, and uses it up at the same time.
And the mechanisms responsible are the same ones responsible for many things that involve desire, learning, reward seeking, and compulsive behavior—including the so-called behavioral addictions like overeating and compulsive sex. However, “the severe consequences of addiction don’t make it a disease, any more than the consequences of violence make violence a disease.”
In an email exchange after the conference, I followed up with Dr. Lewis on some of these matters, and he sent me the following additional thoughts on the “diseasing” of addiction:
Proponents of the disease model argue that addiction changes the brain. And they're right: it does. But the brain changes anyway, at every level, from gene expression, to cell density, to the size and shape of the cortex itself. Of course, neuroscientists who subscribe to the disease model must know that brains change over development. Their take on pathological brain change would have to be very specific in order to be convincing. For example, they would have to show that the kind (or extent or location) of brain change characteristic of addiction is nothing like that observed in normal learning and development. But this they cannot do. The kind of brain changes seen in addiction also show up when people take up rock collecting, fall in love, learn how to cook, or become obsessed with their appearance. The brain contains only a few major traffic routes for learning and goal seeking. And, like the main streets of a busy city, they are often under construction. Brain disease may be a useful metaphor for how addiction seems, but it's not a valid explanation for how it actually works.
Wednesday, December 18, 2013
What Mark Kleiman Wants You To Know About Drugs
The public policy guru guiding state legalization efforts.
Mark A. R. Kleiman is the Professor of Public Policy at UCLA, editor of the Journal of Drug Policy Analysis, author of many books, and generally regarded as one of the nation’s premier voices on drug policy and criminal justice issues. Mr. Kleiman provides advice to local, state, and national governments on crime control and drug policy. When the state of Washington needed an adviser on the many policy questions they left unanswered with the passage of I-502, which legalized marijuana in that state, they turned to Kleiman.
In the past two years, Kleiman has co-authored to Q and A-style books: Drugs and Drug Policy: What Everyone Needs to Know (2011) with Jonathan P. Caulkins and Angela Hawken; and Marijuana Legalization: What Everyone Needs to Know (2012) with Hawken, Caulkins, and Beau Kilmer.
Here, excerpted from the two books, is a brief sampling of Kleiman and his colleagues on a variety of drug and alcohol issues.
Is marijuana really the nation’s leading cash crop?
“Alas, the facts say otherwise. Analyses purporting to support the claim must contort the numbers, citing the retail price of marijuana but the farmgate price of other products, or pretending that all marijuana consumed in the United States is sinsemilla, or ignoring the fact that most marijuana used in the United States is imported, or simply starting with implausible estimates of U.S. production…. marijuana [is] in the top fifteen, but not the top five, cash crops, ranking somewhere between almonds and hay, and perhaps closest to potatoes and grapes.”
How much drug-related crime, violence, and corruption would marijuana legalization eliminate?
“Not much…. Eighty-nine percent of survey respondents report obtaining marijuana most recently from a friend or relative, and more than half (58 percent) say the obtained it for free. That stands in marked contrast to low-level distribution of heroin and crack which often occurs in violent, place-based markets controlled by armed gangs.”
How much would legal marijuana cost to produce?
“The punch line is that full legalization at the national level—as opposed to only legalizing possession and retail sale—could cut production costs to just 1 percent of current wholesale prices…. This would make legal marijuana far and away the cheapest intoxicant on a per-hour basis.”
How would legalization affect me if I’m a marijuana grower?
“It would almost certainly put you out of business. At first glance, legalization might seem like a great opportunity for you…. But legalization will completely upend your industry, and the skills that made you successful at cultivating illegal crops will not have much value. A few dozen professional farmers could produce enough marijuana to meet U.S. consumption at prices small-scale producers couldn’t possibly match. Hand cultivators would be relegated to niche markets for organic or specialty strains.”
Would marijuana regulations and taxes in practice approach the public health ideal?
“If there is a licit, for-profit marijuana industry, one should expect its product design, pricing, and marketing actions to be designed to promote as much frequent use and addiction as possible. Efforts to tax and regulate in ways that promote public health would have to contend with an industry mobilizing its employees, shareholders, and consumers against any effective restriction. Since the industry profits from problem users, we should expect that lobbying effort to be devoted to blocking policies that would effectively control addiction. The alcohol and tobacco industries provide good examples.”
Can we persuade children not to use drugs?
"Even the best prevention programs have only modest effects on actual behavior, and may programs have no effect at all on drug use…. Anesthesiologists know far more about drugs and drug abuse than could possibly be taught in middle-school prevention programs; nonetheless, they have high rates of substance abuse, in part because they have such easy access.”
Why is there a shortage of drug treatment?
“Some specific categories—especially those in need of residential care, and more especially mothers with children in need of residential care—face chronic shortages. But if we had enough capacity for all those who need treatment, many of those slots would be empty because not all the people who ought to fill them want treatment.”
How much money is involved?
“Most of the numbers about drug abuse and drug trafficking that officials peddle to credulous journalists are little better than fiction. Estimates of hundreds of billions of dollars per year in international drug trade—which would make it comparable to food, oil, and arms—do not have a basis in the real world. The most recent serious estimate of the total retail illicit drug market in the United States—by all accounts the country whose residents spend the most on illicit drugs—puts the figure at about $65 billion.”
When it comes to drugs, why can’t we think calmly and play nice?
“American political analysts talk about ‘wine-track (college-educated) and ‘beer track’ (working-class) voters…. So the politics of drug policy is never very far from identity politics…. The notion that illicit drug taking is largely responsible for the plight of minorities (and of poor people generally) and that income-support programs have the perverse consequence of maintaining drug habits has been a staple of a certain form of American political rhetoric at least since Ronald Reagan.”
Are we stuck with our current alcohol problem?
"By no means…. tripling the tax would raise the price of a drink by 20 percent and reduce the volume of drinking in about the same proportion. Most of the reduced drinking would come from heavy drinkers, both because they dominate the market in volume terms and because their consumption is more price-sensitive…."
Sunday, September 22, 2013
Do Addicts Benefit From Chronic Care Management?
Controversial JAMA study questions orthodox addiction treatment.
What is the best way to treat addiction? The conventional wisdom has been to treat it with chronic care management (CCM), the same approach used for various medical and mental illnesses. But a study in the Journal of the American Medical Association (JAMA) purports to demonstrate that “persons with alcohol and other drug dependence who received chronic care management (CCM)” were no more likely to become abstinent that those who received nothing beyond a timely appointment with a primary care physician, and a list of addiction treatment resources.
563 patients were divided into a chronic care management group and a primary care group. The chronic care management group received extended care under a primary care physician, plus
“motivational enhancement therapy; relapse prevention counseling; and on-site medical, addiction, and psychiatric treatment, social work assistance, and referrals (to specialty addiction treatment mutual help.)” The primary care group got the aforementioned doctor’s appointment and printed list of treatment resources.
The study by researchers at Boston Medical Center found that “there was no significant difference in abstinence from opioids, stimulants, or heavy drinking between the CCM (44%) and control (42%) groups. No significant differences were found for secondary outcomes of addiction severity, health-related quality of life, or drug problems.”
But there are limitations. To wit:
1) Small sample size. 282 patients in a Boston Hospital’s chronic care management facility, and 281 participants farmed out to a primary care physician, is the total. Given the known failure rates for chronic care management as applied to smoking, diabetes, and mental illness, and variability in the counseling given the control group by individual physicians, 563 people isn’t really a sufficient cohort to be anything but suggestive. And, since many alcoholics and other drug addicts get sober by means of their own efforts, independent of formal medical intervention, percentage comparisons of such small groups are problematic in addiction studies.
2) Hard Core Cases Only. “Most study participants were dependent on both alcohol and other drugs, recruited from a detoxification unit, had substantial mental health symptoms had recently been homeless, and were not necessarily seeking addiction treatment,” according to the JAMA study. Okay, who might the findings not apply to? “Addiction treatment-seeking or less severely affected populations or to populations recruited elsewhere.”
3) Mostly self-reported data. The investigators assessed main outcomes by self-report. “Biological tests are inadequate for detecting substance use, particularly when it is not recent,” they explain. “Substance use problems and health-related quality of life are best assessed by self-report.” Outcomes were also based on self-reported 30-day abstinence.
4) Alcohol abusers did better under CCM. The research documented “a small effect on alcohol problems among those with dependence.” On alcoholics, in other words. “No subgroup effects were found except among those with alcohol dependence, in whom CCM was associated with fewer alcohol problems.” So CCM works, at least to a degree, for alcoholics, even in this study. Nonetheless, the study concludes: “CCM for substance dependence in primary care is not effective, at least not as implemented in this study and population.” (Note the caveats, and see #2 above)
5) Treatment fails for many reasons. One reason might be that the length of treatment was too short. According to the study, the intervention group “had, on average, 6 CCM visits….” Moreover, “the whole group improved over time; the change most likely was due to many participants having been enrolled at a detoxification unit….” The researchers also admit that “assessment effects in treatment trials are inconsistent and poorly understood and often absent in studies of people not seeking treatment.”
It may even be true that chronic care management, which seems so logical and successful an approach for everything from depression to smoking cessation, doesn’t work any better for drug addiction than a simple doctor’s visit and a handful of pamphlets. But this study doesn't clinch the case.
Graphics Credit: http://www.ihi.org
Saitz R. (2013). Chronic Care Management for Dependence on Alcohol and Other Drugs: The AHEAD Randomized Trial
Sunday, March 24, 2013
More Hard Facts About Addiction Treatment
“Yes, we take your insurance.”
Recent reportage, such as Anne Fletcher’s book, Inside Rehab, has documented the mediocre application of vague and questionable procedures in many of the nation’s addiction rehab centers. You would not think the addiction treatment industry had much polish left to lose, but now comes a devastating analysis of a treatment industry at “an ethics crossroads,” according to Alison Knopf’s 3-part series in Addiction Professional. Knopf deconstructs the problems inherent in America’s uniquely problematic for-profit treatment industry, and documents a variety of abuses. We are not talking about Medicaid, Medicare, or Block Grants here. Private sector dollars, Knopf reaffirms, do not “guarantee that the treatment is evidence-based, worth the money, and likely to produce a good outcome.” Even Hazelden, it turns out, is prepared to offer you “equine therapy,” otherwise known as horseback riding.
Knopf, who is editor of Alcoholism and Drug Abuse Weekly, was specifically looking at private programs, paid for by insurance companies or by patients themselves. Who is in charge of enforcing specific standards of business practice when it comes to private drug and alcohol rehabs? Does the federal government have some manner of regulatory control? According to a physician with the Substance Abuse and Mental Health Services Administration (SAMHSA), the feds rely on the states to do the regulating. And according to state officials, the states look to the federal agencies for regulatory guidance.
All too often, the states routinely license but do not effectively monitor treatment facilities, or give useful consumer advice. Florida state officials do not even know, with any certainty, exactly how many treatment centers are in operation statewide. And even if state monitoring programs were effective and aggressively applied, “just because something is legal doesn’t mean it’s ethical,” said the SAMHSA official.
“We see this as a pivotal time for the treatment field as we have come to know it,” said Gary Enos, editor of Addiction Professional, in an email exchange with Addiction Inbox. Enos said that “the Affordable Care Act (ACA) will move addiction treatment more into the mainstream of healthcare, and this will mean that treatment centers' referral and insurance practices will come under more scrutiny than ever before.”
Among the questionable practices documented by Knopf:
—Paying bounties and giving gifts to interventionists in return for client referrals.
Under Medicare, paying interventionists for referrals is banned. “In the private sector,” says a California treatment official, “it’s not illegal. But it is unethical.” According to treatment lobbyist Carol McDaid, “kickbacks happen all the time. Treatment centers that are doing this will do so at their own peril in the future,” she told Knopf.
—Giving assurances that treatment will be covered by insurance even though only a portion of the cost is likely to be covered.
Under the Affordable Care Act (ACA), says the SAMHSA official, “We are trying to position people to know more about their benefit package. And the industry has to be more straightforward about what the package will cover.” John Schwarzlose, CEO of the Betty Ford Center, told Knopf that “it’s very hard for ethical treatment providers to compete against insurance bait-and-switch,” when patients are told their insurance is good—but aren’t told that the coverage ends after 7 days, or that the daily maximum payout doesn’t meet the daily facility charges.
—Billing patients directly for proprietary nutrient supplements, brain scans, and other unproven treatment modalities.
“Equine therapy, Jacuzzi therapy, those are nice things, and maybe they help with the process of engagement,” said one therapist. “But people need to recognize that these ancillaries aren’t the essence of getting sober.”
—Engaging in dubious Internet marketing schemes.
You see them on the Internet: dozens and dozens of addiction and rehab referral sites. They list private services in various states, and look, on the surface, like legitimate information resources for people in need. As the owner of a blog about drugs and addiction, I hear from them constantly, asking me for links. “Family members and patients frequently have no way of knowing that a treatment program was really a call center they got to by Googling ‘rehab,’ writes Knopf, “and that the call center gets paid for referring patients to the actual treatment center. They don’t know that a program that promises to ‘work with’ health insurance knows full well the insurance will cover only a few days at the facility, and the rest will have to be paid out of pocket.” She points to a 2011 Wired magazine article, which said the Internet marketing cost of key words like “rehab” and “recovery” can be stratospheric. But “by spending that money—not necessarily providing good service—treatment provides can come out on top on searches. It’s the new marketing to the desperate.”
The group with the most to lose from revelations of this nature is the National Association of Addiction Treatment Providers (NAATP), the association representing both private and non-profit rehab programs. The Betty Ford Center has discontinued its membership in NAATP, a move that reflects the turmoil of the industry today. “It’s crazy that we have treatment centers inviting interventionists and other referents on a cruise, and then giving everyone an iPad,” Schwarzlose said.
As one man who lost his son to an overdose said: “I don’t get it. There’s the American Cancer Society, but I look for drugs and alcohol and I can’t find anything. There’s no National Association for Addictive Disease. How can this be?”
The investigative series will be featured in Addiction Professional’s March/April print issue. Enos believes that “influential treatment leaders are more interested than ever to see this debate aired more publically,” and says that the online publication of Knopf’s articles for the magazine has sparked “a great deal of discussion in treatment centers and on social media, including comments about other questionable practices that harm the field’s reputation.”
Tuesday, February 26, 2013
Addiction Rehab: Everything is Broken
Down the rabbit hole in search of effective treatment.
When I first began researching drugs and addiction years ago, a Seattle doctor told me something memorable. “It’s as if you had cancer,” she said, “and your doctor’s sole method of treatment consisted of putting you in a weekly self-help group.”
I’ve got nothing against weekly self-help groups, to be sure. But as Ivan Oransky, executive editor of Reuters Health and a blogger at Retraction Watch, told me as recently as least year, addiction treatment appeared to be “all selling and self-diagnosis. They’re selling you on the fact that you need to be treated.”
In his introduction to Inside Rehab by Anne M. Fletcher (pictured), treatment specialist and former deputy drug czar A. Thomas McLellan writes that the book is “filled with disturbing accounts of seriously addicted people getting very limited care at exhaustive costs and with uncertain results...”
A common notion about addiction treatment facilities, or rehabs, is they are commonly called, is that they are staffed by professional social workers, certified counselors, and family psychologists, as well as addiction specialists. However: “Of the twenty-one states that specify minimum educational requirements for program or clinical directors of rehabs, only eight require a master’s degree and just six require credentialing as an addiction counselor,” writes Fletcher. Neuroscience journalist Maia Szalavitz, who writes for Time Healthland and specializes in addiction and rehab, told Fletcher that “the addiction field has been about as effectively regulated as banking before the economic crisis in many states.” According to Tom McLellan, counselor and director turnover in addiction treatment programs is “higher than in fast-food restaurants.”
In the United States, where for-profit treatment is prevalent, money does not buy access to superior treatment. Fletcher, author of several self-help books on weight loss and alcoholism, doggedly documents what she learns from visiting treatment facilities and interviewing current and former staff and clients. One difficulty with a book of this kind, based primarily on first-hand accounts, is that the same treatment program can offer vastly contrasting experiences from one client to another. And Fletcher, no fan of the 12 Steps, wants AA and NA to account for themselves in a way those volunteer institutions were never designed to accomplish.
But let’s just say it: Addiction treatment in America is a disaster. Addicts get better despite the treatment industry as often as they get better because of it. How did it all go wrong? Part of the answer is that addiction, like depression, tuberculosis, and other chronic conditions, is a segregated illness, as McLellan explains in his introduction. Traditionally, chronic conditions like alcoholism “were not recognized as medical illnesses, and have only recently been taught in most medical schools and treated by physicians. They were seen as ‘lifestyle problems’ and care was typically provided by concerned, committed individuals or institutions not well connected to mainstream health care.”
For treatment of alcoholism and drug addiction, the work has historically fallen to addicts themselves, due to discrimination, segregation, and stigmatization. This prevailing condition is still seen today in many group treatment programs, which are often administered in large part by former addicts with little or no formal training, rather than medical or psychological professionals. Addiction, as the author’s husband wryly remarked, “is the only disease for which having it makes you an expert.”
Which brings up a central point: Where are all the M.D.s? Doctors aren’t helping, either, when they fail to screen for risky drinking or drug use, or when they automatically refer addicts rather than treating them.
If Christopher Kennedy Lawford’s new book, Recover to Live, is the pretty picture, then Fletcher’s Inside Rehab is the gritty picture, in which most addicts who recover don’t go to treatment, 28 days is not long enough to accomplish anything but detox, group counseling is not always the best way to treat addiction, the 12 Steps are not always essential to recovery, specialty drugs are often needed to treat drug addiction, and, perhaps the most troubling of all, most addiction programs do not offer state-of-the-art approaches to treatment that have been shown to be effective in scientific studies.
What clients get, for the most part, is “group, group, and more group,” Fletcher writes. And in many cases of residential or outpatient rehab, “the clients did most of the therapy.” The scientific evidence suggests that some addicts do better with an emphasis on individual counseling, rather than the constant reliance on group work that traditional rehabs have to offer. As one counselor put it: “If I made an appointment to see a therapist because I was depressed, would I be told I have to do a program with everyone else?”
Monthly residential treatment can easily cost $25,000 or more. But public, government funded rehab centers, which presumably have less incentive to treat clients like money, are frequently full. And since these programs run the bulk of prison-related treatment in this country, addicts often stand a better chance of getting into these less expensive programs if they commit a crime.
Even if you manage to get in, rehab rules all too often seem arbitrary and punitive: Recreational reading materials, musical instruments, cell phones, and computers are frequently not permitted. And there is a strong tendency to insist that use equals abuse in every circumstance. Rehab management—the business of what happens after formal treatment ends—is largely neglected in the treatment sphere.
Fletcher rails against the disease model, but mostly in response to how she believes this concept is presented by AA/NA. Like other critics, she dwells on the idea that the disease tag serves as a crutch and an excuse, rather than as an extremely empowering notion for many addicts. In fact, the disease model, as addiction scientists understand it, is seriously underrepresented in the treatment field. Too many mental health professionals continue to insist that “all you need to do is get to the bottom of the problem and the need to use substances to cope, will dissipate,” said an M.D. specializing in addiction. “However, there is absolutely no evidence that this approach works for people who are addicted to alcohol or drugs… The primary-secondary issue is moot and an artifact of the bifurcation of the treatment delivery system.”
A significant number of rehabs still oppose medication-assisted treatment, Fletcher makes clear. Hazelden made news recently for dropping its long-standing opposition to buprenorphrine as a maintenance drug for opiate addicts during treatment. Richard Saitz of Boston University’s School of Medicine says in the book that if addiction were viewed like other health problems, “patients addicted to opioids who are not offered the opportunity to be on maintenance medications would sue their providers and win.”
According to Dr. Mark Willenbring, former director of the National Institute on Alcohol Abuse and Alcoholism (NIAAA): “No one wants to say, ‘Treatment as we’ve been doing it probably isn’t as effective as we thought, and we need more basic research to really come up with new tools. In the meantime let’s do what we can to help suffering people in the most cost effective way and strive to not harm them.’”
Sunday, February 24, 2013
How to Kick Everything
Christopher Kennedy Lawford on recovery.
Christopher Kennedy Lawford’s ambitious, one-size-fits-all undertaking is titled Recover to Live: Kick Any Habit, Manage Any Addiction: Your Self-Treatment Guide to Alcohol, Drugs, Eating Disorders, Gambling, Hoarding, Smoking, Sex, and Porn. That pretty much covers the waterfront, and represents both the strengths and the weaknesses of the book.
There’s no doubting Lawford’s sincerity, or his experiential understanding of addiction, or the fact that the raw ingredients were present in his case: bad genes and a traumatic early environment. He is related to Ted Kennedy, two of his uncles were publically murdered, and he started using drugs at age 12. But this book doesn’t dwell on his personal narrative. Lawford is a tireless supporter of the addiction recovery community, and Recover to Live is meant to be a one-stop consumer handbook for dealing with, as the title makes clear, any addiction.
To his credit, Lawford starts out by accurately pegging the addiction basics: A chronic brain disorder with strong neurological underpinnings. He cites a lot of relevant studies, and some questionable ones as well, but ultimately lands on an appropriate spot: “You can’t control which genes you inherited or the circumstances of your life that contributed to your disease. But once you know that you have the disease of addiction, you are responsible for doing something about it. And if you don’t address your problem, you can’t blame society or anyone in your life for the consequences. Sorry. That’s the way it works.”
Once you know, you have to treat it. “It can turn the most loving and nurturing home into a prison of anger and fear,” Lawford writes, “because there is no easy fix for the problem, and that infuriates many people.”
Lawford includes good interviews with the right people—Nora Volkow, Herb Kleber, and Charles O’Brien among them. And he makes a distinction frequently lost in drug debates: “Nondependent drug use is a preventable behavior, whereas addiction is a treatable disease of the brain.” Due to our penchant for jailing co-morbid addicts, “our prisons and jails are the largest mental health institution in the world.” He also knows that hidden alcoholism and multiple addictions mean “rates of remission from single substances may not accurately reflect remission when viewed broadly in terms of all substances used.”
One nice thing about Lawford’s approach is that he highlights comorbidity, the elephant in the room when it comes to addiction treatment. Addiction is so often intertwined with mental health issues of various kinds, and so frequently left out of the treatment equation. The author is correct to focus on “co-occurring disorders,” even though he prefers the term “toxic compulsions,” meaning the overlapping addictions that can often be found in the same person: the alcoholic, chain-smoking, compulsive gambler being the most obvious example.
The curious inclusion of hoarding in Lawford’s list of 7 toxic compulsions (the 7 Deadly Sins?) is best explained by viewing it as the flipside of compulsive shoplifting, a disorder which is likely to follow gambling into the list of behavioral dependencies similar to substance addictions. In sum, writes Lawford, “If we are smoking, overeating, gambling problematically, or spending inordinate amounts of time on porn, we will have a shallower recovery from our primary toxic compulsion.” Lawford sees the exorcising of childhood trauma as the essential element of recovery—a theory that has regained popularity in the wake of findings in the burgeoning field of epigenetics, where scientists have documented changes in genetic expression beyond the womb.
But in order to cover everything, using the widest possible net, Lawford is forced to conflate an overload of information about substance and behavioral dependencies, and sometimes it doesn’t work. He quotes approvingly from a doctor who tells him, “If you’re having five or more drinks—you have a problem with alcohol.” A good deal of evidence suggests that this may be true. But then the doctor continues: “If you use illicit drugs at all, you have a problem with drugs.” Well, no, not necessarily, unless by “problem” the doctor means legal troubles. There are recreational users of every addictive substance that exists—users with the right genes and developmental background to control their use of various drugs. And patients who avail themselves of medical marijuana for chronic illnesses might also beg to differ with the doctor’s opinion.
Lawford attempts to rank every addiction treatment under the sun in terms of effectiveness (“Let a thousand flowers bloom”), an operation fraught with pitfalls since no two people experience addictive drugs in exactly the same way. Is motivational enhancement better than Acamprosate for treatment of alcoholism, worse than cognitive therapy, or about as good as exercise? Lawford makes his picks, but it’s a horse race, so outcomes are uncertain. Moderation management, web-based personalized feedback, mindfulness meditation, acupuncture—it’s all here, the evidence-based and the not-so-evidence based. Whatever it is, Lawford seems to think, it can’t hurt to give it a try, and even the flimsiest treatment modalities might have a calming effect or elicit some sort of placebo response. So what could it hurt.
Lawford’s “Seven Self-Care Tools” with which to combat the Seven Toxic Compulsions vary widely in usefulness. The evidence is controversial for Tool 1, Cognitive Behavioral Therapy. Tool 2, 12-Step Programs, is controversial and not to everybody’s taste, but used as a free tool by many. Tool 3 is Mindfulness, which is basically another form of cognitive therapy, and Tool 4 is Meditation, which invokes a relaxation response and is generally recognized as safe. Tool 5, Nutrition and Exercise, is solid, but Tool 6, Body Work, is not. Treatments like acupuncture, Reichian therapy, and other forms of “body work” are not proven aids to addicts. Tool 7, Journaling, is up to you.
One of the more useful lists is NIDA director Nora Volkow’s “four biggest addiction myths."
First: “The notion that addiction is the result of a personal choice, a sign of a character flaw, or moral weakness.”
Second: “In order for treatment to be effective, a person must hit ‘rock bottom.’”
Third: “The fact that addicted individuals often and repeatedly fail in their efforts to remain abstinent for a significant period of time demonstrates that addiction treatment doesn’t work.”
Fourth: “The brain is a static, fully formed entity, at least in adults.”
Finally, Lawford puts a strong emphasis on an important but rarely emphasized treatment modality: brief intervention. Why? Because traditional, confrontational interventions don’t work. The associate director of a UCLA substance abuse program tells Lawford: “I haven’t had a drink now in 25 years, and this doctor did it without beating me over the head with a big book, without chastising me, or doing an intervention. What he did was a brief intervention. Health professionals who give clear information and feedback about risks and about possible benefits can make a huge difference. A brief intervention might not work the first time. It might take a couple of visits. But we need more doctors who know what the symptoms of alcohol dependence are and know what questions to ask.”
If your knowledge of addiction is limited, this is a reasonable, middle-of-the-road starting point for a general audience.
Wednesday, July 25, 2012
Broken Treatment: How the Addiction Industry is Failing its Clients
It’s not medical. It's not psychiatric. What is it?
1. Most clinicians who treat addicted patients are counselors, not physicians; thus they cannot prescribe medication and they generally don’t “believe” in the use of medication for addictive disorders.
2. Most patients have medical insurance that excludes or severely limits treatment of addictive disorders, so payment for service is not good. This situation may change in the near future with the advent of healthcare reform in the United States.
So writes Dr. Charles O’Brien of the University of Pennyslvania Perelman School of Medicine, in a recent article for The Dana Foundation’s website. In his article—“If Addictions Can Be Treated, Why Aren’t They?”—Dr. O’Brien asks a basic question: “Why are most patients not even given a trial of medication in most respected treatment programs?”
Even though pharmaceutical companies have throttled back on their interest in anti-craving drugs in recent years, there are, in fact, a few medications recognized by the FDA, primarily for use in the treatment of alcoholism. But they are not much in favor, and O’Brien believes he knows why:
The answer seems to be that there is a bias among treatment professionals, perhaps passed down from past generations when addictions were not understood to be a disease. Medically trained personnel are minimally involved in the addiction treatment system and most medical schools teach very little about addiction so most physicians are unaware of effective medications or how to use them.
What is on offer at most addiction treatment facilities is not actual rehabilitation, but rather short-term detoxification. And what we’ve learned from neuroscience is that taking away the drug is only stage one. The addiction remains, the reward and memory systems still operating erratically. We understand some of this circuitry better than at any time in history, but the concrete effects of these insights at the level of the community treatment clinic have been small to nonexistent. Money, of course, is part of it, since addiction has only recently, and sporadically, gotten the attention of funding agencies in the public health community.
Health journalist Maia Szalavitz, writing at Time Healthland concurs: “Unlike most known diseases, the treatment of addiction is not based on scientific evidence nor is it required to be provided by people with any medical education—let alone actual physicians—according to a new report.” The report in question, from Columbia University’s National Center on Addiction and Substance Abuse (CASA), notes that most people are shoehorned into a standardized approach built around the 12 Step model of Alcoholics Anonymous. “The dominance of the 12-step approach,” writes Szalavitz, “also leads to a widespread opposition to change based on medical evidence, particularly the use of medications like methadone or buprenorphine to treat opioid addictions—maintenance treatments that data have show to be most effective.”
Szalavitz also believes she knows why, and her thinking is similar to O’Brien’s. “Other medications that are known to treat alcohol and drug addiction, such as naltrexone, are also underutilized,” she writes, “while philosophical opposition to the medicalization of care slows uptake.”
There is a straightforward reason for considering the use of medication in the treatment of addiction: strong suggestions of recognizable genetic differences between those who respond to a given medication, and those who don’t. As O’Brien explains, a prospective study now in progress will be looking to see if alcoholics with a specific opioid receptor variant show a better outcome on naltrexone than those with the standard gene for that opioid receptor. And if they do, the FDA may allow a labeling change “stating that alcoholics with this genotype can be expected to have a superior response to naltrexone.”
But that won’t be happening tomorrow. In the meantime, we are stuck with the addiction treatment industry as it is. “The [CASA] report notes that only 10% of people with substance-use problems seek help for them,” Szalavitz concludes. “Given its findings about the shortcomings of the treatment system, that’s hardly surprising.”
Photo Credit: Creative Commons
Saturday, July 21, 2012
John Berryman and the Poetry of “Irresistible Descent”
“The penal colony’s prime scribe.”
“Will power is nothing. Morals is nothing. Lord, this is illness.”
—John Berryman, 1971
A year before he committed suicide by jumping off a Minneapolis bridge in 1972, Pulitzer Prize-winning poet John Berryman had been in alcohol rehab three times, and had published a rambling, curious, unfinished book about his treatment experiences. Recovery is a time capsule. If you think we have little to offer addicts by way of treatment these days, consider the picture in the 60s and 70s. In Recovery, treatment consists almost entirely of Freudian group analysis, and while there is regular talk of alcoholism as a disease, AA style, there is no evidence that it was actually dealt with in this way, after detoxification.
Best known for “Dream Songs,” Berryman taught at the University of Minnesota, and was known as a dedicated if irascible professor. Scientist Alan Severence, Berryman’s stand-in persona in the book, comes into rehab hard and recalcitrant, despite his previous failures: “Screw all these humorless bastards sitting around congratulating themselves on being sober, what’s so wonderful about being sober? Great Christ, most of the world is sober, and look at it!” And he is suffering from “the even deeper delusion that my science and art depended on my drinking, or at least were connected with it, could not be attacked directly. Too far down.”
Berryman was a difficult man, and knew it. He quotes F. Scott Fitzgerald: “When drunk, I make them pay and pay and pay and pay.”
Alcoholics, writes Berryman, are “rigid, childish, intolerant, programmatic. They have to live furtive lives. Your only chance is to come out in the open.” Berryman catches the flavor of group interaction after too many hours, too much frustration, and too much craving. One inpatient lashes out: “You’re lying when you say you do not do anything about your anger. You get bombed. It is called medicating the feelings, pal. Every inappropriate drinker does it. Cause and effect. Visible to a child. Not visible to you.”
Berryman was a shrewd observer, a singular writer, and, after all, a poet. He is extraordinary on the subject of alcoholic dissociation: “I found myself wondering whether I would turn off right towards the University and the bus home or whether I would just continue right on to the Circle and up right one block to the main bar I use there, and have a few. Wondering. My whole fate depending on pure chance…. as if one were not even one’s own actor but only a spectator.”
Berryman puts it all together in a horrific capsule description of the “irresistible descent, for the person incomprehensibly determined.”
Relief drinking occasional then constant, increase in alcohol tolerance, first blackouts, surreptitious drinking, growing dependence, urgency of FIRST drinks, guilt spreading, unable to bear discussion of the problem, blackout crescendo, failure of ability to stop along with others (the evening really begins after you leave the party)… grandiose and aggressive behavior, remorse without respite, controls fail, resolutions fail, decline of other interests, avoidance of wife and friends and colleagues, work troubles, irrational resentments, inability to eat, erosion of the ordinary will, tremor and sweating… injuries, moral deterioration, impaired and delusional thinking, low bars and witless cronies….
Berryman had no illusions about his failed attempt to hide behind the mask of a social drinker: “It seems to be loss of control. Unpredictability. That’s all. A social drinker knows when he can stop. Also, in a general way, his life-style does not arrange itself around the chemical, as ours does. For instance, he does not go on the wagon…”
In the end, he was "pleading the universal case of hope for abnormal drinkers, for all despairing and deluded sufferers fighting for their sanity in a world not much less insane itself and similarly half-bent on self-destruction…”
As the head nurse in the facility tells the group: “You are all suffering from the lack of self-confidence… often so powerful that it leads to consideration of suicide, a plan which if adopted will leave you really invulnerable, quite safe at last.”
And as Saul Bellow wrote in the introduction to Recovery: “At last there was no more. Reinforcements failed to arrive. Forces were not joined. The cycle of resolution, reform and relapse had become a bad joke which could not continue.” Berryman agreed. Toward the end, he wrote: “I certainly don’t think I’ll last much longer.”
“There’s hope until you’re dead,” a woman tells him during his final stay in rehab. Sadly, that hope ended a few months later.
Photo posted by Tom Sutpen for the series: Poets are both clean and warm
Tuesday, March 13, 2012
Interview with Deni Carise, Chief Clinical Officer of Phoenix House
Why addiction treatment works—if you let it.
This time around, our “Five-Question Interview” series features clinical psychologist Deni Carise, senior vice president and chief clinical officer at Phoenix House, a leading non-profit drug treatment organization with more than 100 programs in 10 states. Chances are, you may have seen or heard her already: Dr. Carise has been a guest commentator about drugs and addiction for Nightline, ABC’s Good Morning America, Fox News, and local New York media outlets. She is frequently quoted in US News and World Report and other periodicals, blogs at Huffington Post, and has also consulted for the U.N. Office on Drugs and Crime.
Dr. Carise earned her doctorate at Drexel University, and served as a post-doctoral fellow at the Center for Studies of Addiction at the University of Pennsylvania. Currently, she is also adjunct clinical professor in the University of Pennsylvania’s Department of Psychiatry. She has been involved with drug abuse treatment and research for more than 25 years, and has worked extensively in developing countries to integrate science-based drug treatments into local programs. She has worked with adults and adolescent populations including dually diagnosed clients, Native Americans, and with medical populations (including spinal cord-injured, cardiac care and trauma patients).
1. As chief clinical officer for Phoenix House Foundation, what's your job description?
Deni Carise: My main responsibility is to ensure that we provide the highest possible standard of care. This means making sure that treatment methods across our programs are consistent with the latest research, represent a variety of evidence-based practices, and are delivered with fidelity. I also collaborate on the implementation and evaluation of Phoenix House’s national and regional strategies to achieve clinical excellence. My home base is New York, but I work directly with all of our programs and regularly travel to our California, New England, Mid-Atlantic, Texas, and Florida regions. I also oversee the activities of our Family Services, Quality Assurance, Research, Workforce Development, and Training initiatives. Finally, I help Phoenix House spread awareness to the public about the need to reduce the stigma of addiction and to increase access to treatment services.
2. As a clinical psychologist, how did you become involved in drug and alcohol treatment and recovery?
Deni Carise: I actually became involved in the Substance Abuse Treatment (SAT) field prior to becoming a clinical psychologist. When I decided that I wanted to get sober, I got some help from a counselor. This counselor was so helpful to my recovery that I decided to become an SA counselor so that I could assist others on this journey. I was working as a model at that time, and there were a few aspects of that career that I didn’t like: First, it was very clear that I would become less valuable in my career as I got older; secondly, my value was exclusively based on appearance, not knowledge or skills; and finally, my work didn’t contribute to the greater good—that is, no one benefitted by my work. I wanted a new career where I would become more valuable as I got older and more experienced, and where my knowledge and skills would be of value. I also wanted to do something I felt was contributing to society. The SAT field seemed to fit all these criteria.
3. What makes it so difficult for people to accept the disease components of serious drug addiction?
Deni Carise: People have difficulty accepting the disease concept of addiction for three reasons. First, people believe addiction is self-induced; you wouldn’t have it if you didn’t use drugs, right? There is some truth to this, but of all those who try drugs, an estimated 5 to 10% (depending on the drug) will become addicted. There’s a reason why the other 90 to 95% don’t become addicted.
That brings us to reason #2: People generally don’t believe there is a genetic cause. It is now very clear that there is a genetic component to substance use disorders. For example, if a father is an insulin-dependent diabetic, the heritability estimates range from 70 to 90% likelihood that the man’s son will also be diabetic. For hypertension, the heritability estimates are from 25 to 50%, depending which study we look at. For alcohol, the estimates are 55 to 65% likelihood that a young man will be alcohol dependent if his father is. For opiate dependence, it’s 35 to 50%.
The third and probably most important reason is that people think calling addiction a disease absolves the substance abuser of responsibility for his or her actions. Nothing could be further from the truth. Those in recovery see the disease of alcoholism or addiction as a moral obligation to get well. If you know you have this disease and the only way to keep it under control is not to use alcohol or drugs, then that’s what you have to do.
4. Overall, treatment doesn't seem to be that effective. What's missing?
Deni Carise: I believe treatment is effective. We’re just expecting the wrong results. Substance abuse has the same characteristics as any chronic medical disorder. The problem is that we (society, families, even me) want addiction to respond to treatment as though it’s an acute medical problem, like a broken leg or appendicitis. If it were an acute problem, we could send our kids, loved ones, even ourselves to treatment for a set number of days (maybe 7, maybe 28) and leave the hospital or treatment facility with the condition cured—as we would after surgery for an appendicitis! I would love that.
Unfortunately, we’ve been measuring treatment success the same way we would for a surgical problem, even though substance abuse and dependence are, in fact, chronic problems. Think about this—substance abuse treatment success is often measured by symptoms, drug use, and life problems prior to treatment and again six months after treatment ends. Imagine if we measured success of diabetes treatment the same way. We would measure their blood sugar levels, weight, number of diabetic crises, and other related problems before treatment. Then we’d send them off to a treatment program where we would prescribe medications, maybe give them insulin, teach them about a good diet, discharge them (take away that treatment), and measure their blood sugar levels, weight, etc. six months after we stopped the medication. Do we really think that would work with diabetes? Then why would we think it would work with addiction?
As with all chronic disorders, there are no prolonged, symptom-free periods without continued attention and self-management of the illness. Just as some people with diabetes can manage their illness with behavioral changes such as making healthy decisions when offered cakes or cookies, or starting an exercise program, some people with substance abuse problems can control their symptoms by changing their behaviors. This means not being around others who use, making the right decisions when offered alcohol or drugs, etc. For those who can’t do this alone, there’s treatment to teach them how to manage their disease and there are medications to assist them. And I’m talking about the diabetic and the substance abuser.
So treatment can work, but, just like any chronic disease, there’s no quick fix.
5. You're committed to working with developing countries to bring scientifically valid treatment within reach of poorer populations. How is the effort going?
Deni Carise: I’ve been really lucky to be able to consult for numerous treatment systems, universities, and countries around the world—including training clinicians from Nigeria, Thailand, Egypt, Greece, Iran, Singapore, Brazil, China, Iraq, India, and other countries. It’s fascinating to see how different countries approach local substance abuse problems. Some countries have historically asserted that substance abuse is not a problem in their communities, so for them to offer treatment of any kind means they need to change their socipolitical stance. That doesn’t happen quickly. For one country, the diagnosis of AIDS among 7 substance abusers who had shared needles was the impetus to providing treatment.
Much of what I’ve done internationally involves cultural adaptations of standardized instruments or clinical tools (such as the Addiction Severity Index assessment tool) for use within various cultures. To do this, I typically meet with numerous staff who deliver direct services in the country. We go over each assessment question or worksheet item looking at what would make sense in their culture. Types of things that frequently need adapting are questions about education (not everyone has “high schools”), employment and income, demographic questions such as race categories, and all manner of expressions used to describe drugs and clinical symptoms. Then we pilot the new interview or service with some local clients and get their perspective and make a final version.
Much of this work has been funded by the United Nations Office on Drug Use and Crime, the National Institute on Drug Abuse and Office of National Drug Control Policy.
Subscribe to:
Posts (Atom)