Sunday, July 28, 2013
Crack Babies Are Turning Out Okay
Major study concludes that crack panic was overblown.
In an excellent story for the Philadelphia Inquirer, Susan FitzGerald traces the fortunes of Philadelphia children enrolled in a study that began in 1989, at the height of the crack “epidemic” in the U.S. Headed up by Hallam Hurt, then the chair of neonatology at Albert Einstein Medical Center, a group began the in-vitro study of babies exposed to maternal crack cocaine use. One of the longest-running studies of its kind, the NIDA-funded research on 224 babies born between 1989 and 1992, half of them cocaine-exposed, the other half normal controls, was now coming to a close. And the results were not what most people were expecting.
In the Inquirer article, Hurt notes that cocaine can in fact trigger premature labor, raise blood pressure, and risk a condition in which the placenta breaks loose from the uterine wall. So it was natural to go looking for long-term effects in all of those twitching, underweight newborn crack babies viewers saw on television. Physicians warned that damage to developing dopamine systems would result in long-term or permanent impairments in attention, language, and memory. So Hurt and colleagues went looking—and couldn’t find them. Neither could researchers at other institutions. Said Hurt: “We began to ask, ‘Was there something else going on?’”
As FitzGerald writes: “The years of tracking kids have led Hurt to a conclusion she didn’t see coming. ‘Poverty is a more powerful influence on the outcome of inner-city children than gestational exposure to cocaine,'" Hurt said. For example, babies born to mothers on heroin or methadone will have certain characteristic withdrawal symptoms, which can be managed by informed hospital staff. The same is true with newborns whose mothers have been using crack. In most cases, these withdrawals can be managed without permanent harm to the infant.
In a paper authored by Hurt, Laura M Betancourt, and others, the investigators write: “It is now well established that gestational cocaine exposure has not produced the profound deficits anticipated in the 1980s and 1990s, with children described variably as joyless, microcephalic, or unmanageable.” The authors do not rule out “subtle deficits,” but do not find evidence for them in functional outcomes like school or transition to adulthood.
How did this urban legend get started? In the 1980s, during the Reagan-Bush years, Americans were confronted with yet another drug “epidemic.” The resulting media fixation on crack provided a fascinating look at what has been called “drug education abuse.” This new drug war took off in earnest after Congress and the media discovered that an inexpensive, smokable form of cocaine was appearing in prodigious quantities in some of America’s larger cities. Crack was a refinement to freebasing, and a drug dealer’s dream. The “rush” from smoking crack was more potent, but even more transient, than the short-lived high from nasal ingestion.
Coupled with this development were the cocaine-related deaths of two well-known athletes, college basketball star Len Bias and defensive back Don Rogers of the Cleveland Browns. Bias played for Maryland, a home team in Washington, D.C. Six months earlier, Reagan had brought the military into the drug wars in a major way. The initial test of the directive was Operation Blast Furnace, a no-holds-barred attack on cocaine laboratories in the jungles of Bolivia.
As I wrote in 2008 in The Chemical Carousel:
The death of Len Bias elevated cocaine paranoia to the realm of the mythic. Cocaine became America’s first living-room drug, courtesy of the nightly news. The summer of 1986 will be remembered as the season of the “crack plague,” as viewers were bombarded with long news stories and specials. NBC Nightly News offered a special report on crack, during which a correspondent told viewers: “Crack has become America’s drug of choice... it’s flooding America....”
The hyperkinetic level of television coverage ultimately led TV Guide Magazine to commission a report from the News Study Group, headed by Edwin Diamond at New York University. The investigators quickly demolished the notion that cocaine had become America’s “drug of choice,” and were at a loss to account for where the networks had come up with it: “Statistically, alcohol and tobacco are the legal ‘drugs of choice’: 53 million people smoke cigarettes; 17.6 million are dependent on alcohol or abuse it. Marijuana still ranks as the No. 1 illegal drug. According to NIDA, 61.9 million people in the United States have experimented with marijuana.” The study group went on to note that the often-deadly “Black Tar” heroin had hit the streets of American cities the same summer. “Why was crack a big story [that summer] while Black Tar was not? One reason [is that] crack is depicted as moving into ‘our’—that is, the comfortable TV viewers’—neighborhood.”
Sunday, July 21, 2013
Fruit Fly Larvae Go Cold Turkey and Forget the Car Keys
Not a pretty sight.
Let’s start with the fruit fly, your basic Drosophila. A fruit fly, like a human, can become addicted to alcohol even at a very young age. The larval age. In other words, even as a maggot. And, just like humans, alcohol degrades a fruit fly maggot’s ability to learn. But adaption is an amazing thing, and drunken larvae eventually learn as well as their teetotaling cousins. That is, until the alcohol is taken away, in which case, the maggots become impaired learners once again. The larval nervous system goes haywire, and hyperexcitablity sets in. They can’t concentrate on their work. But one hour of “ethanol reinstatement” restores larval learning to normal levels.
It looks and sounds like withdrawal. Such effects in human alcoholics are often chalked up to state-dependent memory, but neurobiologists at the Waggoner Center for Alcohol and Addiction Research at the University of Texas, whose maggots these are, believe that state-dependent memory is not at work in the case of invertebrate ethanol dependence.
Brooks G. Robinson and associates fed the larvae a 5% ethanol supplement to their daily food. The maggots, incredibly enough, can reach blood-alcohol concentrations as high as 0.08, or roughly the legal limit for humans. If you blew a 0.08, the official chart says you would be suffering from impaired reasoning, disinhibition, and visual disturbances. For the maggots, no different. Larvae that fed on “ethanol food” for one hour learned poorly compared to straight maggots. The learning test, done before introducing alcohol into the picture, used a heat pulse to condition larvae away from an otherwise attractive odor. The reduced attraction to the odor is a form of associative learning. Figuratively speaking, the drunken maggots kept burning themselves on the stove as they reached for the soup. They failed the field sobriety test.
But was it truly a case of impaired learning? Perhaps the drunken larvae had an impaired sense of smell. But the researchers could not document a reduced sense of odor based on responses with untrained animals. And both groups of maggots sensed heat equally, so the reduction in learning was not due to simple alcoholic anesthesia. Could the withdrawal response be due to the fact that alcohol is a calorie-rich food? To test that possibility, the researchers ran the experiment with sucrose instead of alcohol, and didn’t record any learning impairment in that case. As for state-dependent memory, the researchers assert in Current Biology that withdrawal effects “cannot be attributed to state-dependent learning, because the less than 20 minute training and testing assay for all treatment groups occurs on nonethanol plates.”
And finally, the investigators write, “the fact that both the withdrawal-induced learning deficit and the neuronal hyperexcitability responses are reversed by ethanol reinstatement suggests that they have related origins, and that withdrawal learning may suffer because the nervous system is overly excitable.”
So what have we learned? Well, alcohol dependence in humans is clearly associated with learning and memory deficits that can last for a year or more after quitting. Now that the researchers have demonstrated cognitive alcohol dependence in invertebrates—for the first time ever, they say—it may open the door to more sophisticated genetic analyses of alcoholism in Drosophila, for all the reasons that have drawn other biologists to the study of fruit flies over the years.
And there is more research to be done relative to the finding that neuronal hyper-excitability is linked in some way to the learning deficits caused by alcohol. A brief article by Stefan Pulver in the Journal of Experimental Biology notes that the work of Robinson and colleagues “reinforces how eerily conserved ethanol’s physiological effects are across animal taxa. Alcohol addiction is truly the great leveller. It doesn’t matter whether you are man, mouse or maggot—over-consumption of alcohol will trigger very similar cellular and behavioral responses, with devastating consequences.”
Robinson B., Khurana S., Kuperman A. & Atkinson N. (2012). Neural Adaptation Leads to Cognitive Ethanol Dependence, Current Biology, 22 (24) 2338-2341. DOI: 10.1016/j.cub.2012.10.038
Sunday, July 14, 2013
MDPV Turns Lab Rats Into "Window Lickers"
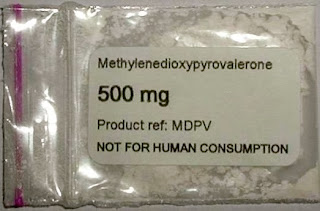 Popular bath salt drug shown to be highly addictive.
Popular bath salt drug shown to be highly addictive. Researchers at the Scripps Research Institute (TSRI) in La Jolla, California, appear to have hammered the last nail into the coffin for the common “bath salt” drug known as MDPV. We can now say with a high degree of certainty that, based on animal models, we know that 3,4-methylenedioxypyrovalerone is addictive—perhaps more strongly addictive than methamphetamine, although such comparisons are always perilous. However, principal investigator Michael A. Taffe, an associate professor at TSRI, said in a prepared release that the research group “observed that rats will press a lever more often to get a single infusion of MPDV than they will for meth, across a fairly wide dose range.”
Like methamphetamine, MDPV works by stalling the uptake of dopamine, and it also has effects on noradrenaline and serotonin. As cathinone derivatives, MPDV and mephedrone are related to the stimulant drug khat, which is used like cocaine in northeastern Africa. In earlier research at Scripps under Dr. Taffe, investigators found that lab rats would intravenously self-administer mephedrone and behave in a manner similar to the effects produced when the rats were on methamphetamine. In a paper for Drug and Alcohol Dependence, the Taffe Lab concluded that “the potential for compulsive use of mephedrone in humans is likely quite high, particularly in comparison with MDMA.”
Now the researchers have zeroed in on the effects of the dirty pharmacology represented by MDPV, the other primary ingredient in many bath salt mixtures. In a new study by Michael Taffe, Tobin J. Dickerson, Shawn M. Aarde, and others, to be published in the August issue of Neuropharmacology, the investigators found that MDPV was a more potent attraction than meth for rats allowed to self-administer the drugs. Very little lab data exists for MDPV, and this study was among the first to directly compare the effect of MDPV to methamphetamine in an animal experiment.
It took some time to tease out the behavioral clues—the cognitive, thermoregulatory, and potentially addictive effects of the drug—but MDPV’s strong affinities with speed can no longer be ignored. The researchers saw the same types of repetitive activities seen in animals on meth, such as excessive grooming, tooth grinding, and skin picking. Lead author Shawn Aarde said in a prepared statement that “one stereotyped behavior that we often observed was a rat repeatedly licking the clear plastic walls of its operant chamber—a behavior that was sometimes uninterruptable.”
MDPV, in the jargon of such experiments, had “greater reward value” than methamphetamine. Which is saying something, given the well-publicized addictive threat of speed. When the group boosted the number of lever presses needed for another infusion of MDPV or meth, “we observed that rats emitted about 60 presses on average for a dose of meth but up to about 600 for MDPV—some rats would even emit 3,000 lever presses for a single hit of MDPV,” said Aarde in a press release. “If you consider these lever presses a measure of how much a rat will work to get a drug infusion, then these rats worked more than 10 times harder to get MDPV.”
Excuse me, did he say as many as three thousand bar presses for another bump of intravenous MDPV? He did. Overall, the rats self-administered more MDPV than methamphetamine. In the paper itself, the authors write that “compared with meth, the effect of MDPV on drug-reinforced behavior was of greater potency (more responding under lowest dose under fixed-ratio schedule) and greater efficacy (more responding under optimal dose under a progressive ratio schedule)…”
The conclusion? MDPV’s “abuse liability” may be greater than that of standard methamphetamine. Which is another excellent piece of evidence for approaching the world of new synthetic psychoactives with great caution.
Aarde S.M., Huang P.K., Creehan K.M., Dickerson T.J. & Taffe M.A. (2013). The novel recreational drug 3,4-methylenedioxypyrovalerone (MDPV) is a potent psychomotor stimulant: Self-administration and locomotor activity in rats, Neuropharmacology, 71 130-140. DOI: 10.1016/j.neuropharm.2013.04.003
Labels:
bath salt,
cathinone,
designer drugs,
MDPV,
mephedrone,
stimulants,
synthetic drugs
Saturday, July 6, 2013
Popular Synthetics: The Class of 2013
Navigating the new alphabet of intoxication.
You don’t have to be a molecular chemist to know which of today’s recreational drugs are safe. Wait, I take that back. You DO have to be a molecular chemist to navigate today’s synthetic drug market with anything like a modest degree of safety.
It’s hard not to get nostalgic: Back in the day, you had your pot, you had your acid, your coke, your speed, and your heroin. And that, with the exception of a few freak outriders like PCP, was about that. Baby boomers of today, already losing touch with leading-edge music—Macklemore? Tame Impala?—can now consider themselves officially out of touch when it comes to illegal drugs.
That is, unless they are familiar with psychoactive chemicals beyond mere methamphetamine “bath salt” knockoffs like mephedrone, and cannabis “Spice” look-alikes such as JWH-018. We’re talking about drugs like Bromo-DragonFly, Benzo Fury, and 2C-B. As Vanessa Grigoriadis writes in New York Magazine: “These drug users imagine themselves as amateur chemists, proto-Walter Whites, sampling and resynthesizing drugs to achieve exactly the state of consciousness they find most pleasurable. And there are no end of drugs to play with.”
A big piece of the synthetic drugs movement can be traced to the work of the legendary Alexander Shulgin, a Harvard grad who worked for Dow chemical, and who invented more than 100 entirely novel hallucinogenic compounds over the years. Other than the hallucinogens investigated by Shulgin and his coterie of personal friends, who were willing to take new hallucinogens and report back, none of the drugs on this list were meant for, or tested on, human beings.
Many of them are not, technically, new. Nonetheless, writes Grigoriadis, "almost every drug, from pot to GHB to morphine, has been messed with, as chemists find that removing a methoxy group or adding a benzene ring makes a new drug with different properties: body-grooving with a side helping of visuals, euphoric or speedy, long or short, or administering just the right dose of primal fear. Formerly known as “designer drugs,” they have morphed into “synthetic highs.” The tricky precursor chemical problem has become much easier to solve in the present moment, when any budding entrepreneur can send the official chemical designation of a drug, called its CAS number, to any of dozens of manufacturers in China, who will provide them with whatever weird “research” drug they need.
Herewith, a sampling of a few popular drugs of the day:
- 2C Series
- Bromo-Dragonfly
- NBOMe Series
- 6-APB (Benzo Fury)
- MDPV
- 5-MeO-DMT
Photo Credit: http://legalmann.wordpress.com/
Labels:
2C-B,
2C-P,
Benzo Fury,
Bromo-Dragonfly,
designer drugs,
DMT,
MDPV,
mephedrone,
Shulgin,
synthetic drugs
Tuesday, June 25, 2013
Addiction Trajectories: Book Review
Striving for that elusive middle ground.
For a journalist who covers neuroscience, the political and psychoanalytic focus of anthropology sometimes feels like a baffling trip to a foreign land. References to Foucault and Derrida abound, and Freud hovers in the middle distance. The investigative landscape is comprised of socially constructed experiences and environmental processes. Trained to seek out cultural and economic experiences as first causes, many cultural anthropologists have been fighting a rear-guard action against the advances of neuroscience for years now. Which is a shame, because anthropology, importantly, can serve to remind medical scientists of the multi-dimensional nature of addiction. “For psychoactive substances to transform themselves into catalysts for and objects of pleasure and desire,” writes anthropologist Anne M. Lovell, “they must circulate not only through blood, brain, and other body sites but also through social settings.”
It is anthropologists, for example, who have documented that “three-fourths of all state-licensed drug treatment programs in Puerto Rico were faith-based.” This study of faith-based healing in the addiction recovery community forms one chapter of a new volume, Addiction Trajectories, edited by Eugene Raikhel of the University of Chicago and William Garriott of James Madison University.
What anthropologists can do for addiction science is document these sociocultural attributes of addiction. In a chapter on buprenorphine and methadone users in New York City and the five boroughs, Helena Hansen, assistant professor of anthropology and psychiatry at New York University, finds that buprenorphine users live in predominantly white, high-income neighborhoods, tended to have college educations, and get their bupe from a private doctor. However, “others are directed to methadone maintenance programs with requirements for daily attendance, urine drug screens, surveillance, and control,” and there is little overlap between the two recovering populations.
There is a chapter devoted to a punitive form of addiction treatment known in Russia as “narcology,” and another that dwells on the semiotics of meth addiction. There are chapters taking drug counselors to task for their inadequate training and lack of nuanced background. And there is a chapter that views the advent of buprenorphine for heroin addiction as a step backwards, or, at best, a typical step sideways—addictive drugs for addiction, just like the old days when heroin addicts were offered alcohol as a cure.
A chapter by E. Summerson Carr is devoted to the treatment known as motivational interviewing, a technique with which she claims “drug users can talk themselves into sobriety regardless of whether or not they originally believe what they say to be true.” Irrespective of your view on M.I., Carr makes a useful point when she notes that sometimes a client’s refusal to admit drug use, even after a positive drug test, is not because of denial, but because of a logical understanding that their status as credible plaintiffs in legal proceedings could be on the line.
And there is simply no arguing Carr’s central point—while addiction science has been increasingly incorporated within the broad outlines of neuroscientific models, “the project of using talk to treat denial and demonstrate insight remains remarkably consistent” in the treatment practices used by the more than 13,000 outpatient addiction treatment programs across the U.S.
What else can anthropologists bring to the table? An understanding of “the loaded institutional and cultural conditions of clinical assessments, which inevitably and profoundly shape what drug users do and do not say.” Chief among these, Carr writes, is “the distinctly clinical terms of addicted denial, the chief organizing heuristic of mainstream American addiction treatment.”
The gap remains wide between addiction viewed as the neuroscientist’s disease entity, and addiction viewed as the anthropologist’s contingent outcome emerging from specific social settings. It’s easy to see why the attempt at an alliance between anthropologists and neurobiologists is an uphill struggle. Reading Addiction Trajectories, it becomes apparent how frequently the two disciplines are talking past one another. But I like to think there are enough bright and motivated anthropologists and neuroscientists around to forge some manner of middle ground; the elusive third way of viewing addiction, holistically, as a living blend of genetic and environmental influences, sensitive to both, and registering that dual sensitivity in the form of compulsive drug taking. (See, for example, anthropologist Daniel Lende’s recent post.)
The more invigorating contributions in this volume help us to zero in on “the popular representation of drugs as inherently criminogenic,” writes William Garriott, as well as the concomitant “lack of faith in the ability of the criminal justice system—and the state more generally—to address drug problems through the punitive management of the addicted offender population.” It is anthropologists, not neuroscientists, who dwell on the ramifications of this paradox: “The majority of Americans appear committed to fighting a war they feel cannot be won, using a strategy in which they no longer believe.”
The present volume is sometimes inclined to view biology with suspicion, and many of its contributors are quick to point out the hazards of attempting to meld social science and neuroscience. A similar but somewhat less skeptical collection—one that seeks to connect the socioenvironmental influences helping to shape how the biological disorder known as addiction will play out in the real world—was published last year by co-editors Daniel H. Lende and Greg Downey. In The Encultured Brain, Lende and Downey look ahead to a time when field-ready equipment will measure nutritional intake, cortisol levels, prenatal conditions, and brain development in the field. Predicting the future is a fool’s game, but it seems clear that the field of anthropology is aware of, and awake to, the controversial research avenues opened up by advances in contemporary neuroscience.
Graphics credit: http://www.culturalneuroscience.org/
Saturday, June 22, 2013
Smoking and Surgery Don’t Mix
Even routine operations are riskier for smokers.
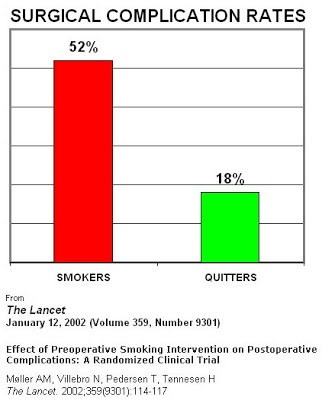
Smokers who are scheduling a medical operation might want to think seriously about quitting, once they hear the results of a new review of the impact of smoking on surgical outcomes.
A scheduled operation is the perfect incentive for smokers to quit smoking. The fact that smokers have poorer post-surgical outcomes, with longer healing times and more complications, is not a new finding. But the study by researchers from the University of California in San Francisco, and Yale University School of Medicine, published in the Journal of Neurosurgery, spells out the surgicial risks for smokers in graphic detail.
Cellular Injury
The systematic effects of nicotine and carbon monoxide in the blood of cigarette smokers result in tissue hypoxia, which is a lack of adequate blood supply caused by a shortage of oxygen. When carbon monoxide floods the bloodstream in high concentrations, as it does in smokers, it is capable of binding with hemoglobin and thus lowering the oxygen-carrying capacity of the blood. A cascade of physiological reactions then lead to the possibility of low coagulation levels, vasoconstriction, spasms, and blood clots.
Wound Healing and Infection
If the circulatory system is dysfunctional, healing will be impaired. “In addition,” the researchers say, “tobacco may stimulate a stress response mediated by enhanced fibroblast activity, resulting in decreased cell migration and increased cell adhesion. The net consequence is inappropriate connective tissue deposition at the surgical site, delayed wound healing, and increased risks of wound infection.”
Blood Loss
In their review of the neurosurgical literature, the researchers found higher blood loss for smokers particularly following surgery for certain kinds of tumors and for lumbar spine injuries. Smoking causes “permanent structural changes of vessels such as vessel wall thickening,” and there is evidence that smoking is linked to “larger and more vascularized tumors, which may further contribute to intraoperative blood loss during resection.”
Cardiopulmonary Effects
Even smokers who don’t have any chronic conditions associated with smoking are at increased risk during and after surgery. Oxidative damage from smoke can cause “mucosal damage, goblet cell hyperplasia, ciliary dysfunction, and impaired bronchial function,” all of which impedes the ability to expel mucus, which increases the bacterial load, which alters the respiratory immune response, and which ultimately leads to higher rates of postoperative pneumonia in smokers.
The authors of the review note that the evidence is particularly strong in certain specialties: Cranial surgery, spine surgery, plastic surgery, and orthopedic surgery. One randomized clinical trial showed that a 4-week smoking cessation program lead to a 50 relative risk reduction for postoperative complications. Another study showed significant improvement in wound healing when patients abstained from smoking for 6 to 8 weeks prior to surgery. And a third trial of smokers cited in the study showed a major decrease in complications following surgery for the repair of acute bone fractures in patients who quit before surgery.
The authors close by suggesting that the seriousness of surgery can be used to create a “teachable moment” for patients who smoke. Other studies show consistently that “patients tend to be more likely to quit smoking after hospitalization for serious illness.” All of this makes the act of scheduling surgery a perfect point of contact with smokers in medical settings. Clinicians can neutrally lay out the facts of the matter, in a way that truly brings home the health consequences of tobacco.
Lau D., Berger M.S., Khullar D. & Maa J. (2013). The impact of smoking on neurosurgical outcomes, Journal of Neurosurgery, 1-8. DOI: 10.3171/2013.5.JNS122287
Graphics Credit: http://www.ontarioanesthesiologists.ca/
Sunday, June 16, 2013
A Weak Smoker’s Vaccine Might Be Worse Than None
New PET scans show wide responses to antibodies.
One of the brightest hopes of addiction science has been the idea of a vaccine—an antibody that would scavenge for drug molecules, bind to them, and make it impossible for them to cross the blood-brain barrier and go to work. But there are dozens of good reasons why this seemingly straightforward approach to medical treatment of addiction is devilishly difficult to perform in practice.
Last January, health care company Novartis threw in the towel on NicVax, a nicotine vaccine that failed to beat placebos in Phase III clinical trials for the FDA. And back in 2010, a report in the Archives of General Psychiatry demonstrated that a vaccine intended for cocaine addicts only generated sufficient antibodies to dull the effects of the cocaine in 38 percent of the test subjects. Moreover, it proved possible to overcome immunization by upping the cocaine dose, which sounded like an invitation to overdose.
And now, neuroscientists at the Society of Nuclear Medicine and Molecular Imaging annual meeting have presented a new study, the conclusions of which might help researchers understand why the vaccine results have been so mixed. The research “represents one of the first human studies of its kind using molecular imaging to test an investigational anti-nicotine immunization,” lead author Alexey Mukhin, professor of psychiatry and behavioral science at Duke University Medical Center, said in a prepared statement.
Subjects underwent two PET brain scan as they smoked nicotine labeled with radioactive C-11, one before the vaccine was administered, and one after. Ten subjects who developed “high-affinity antibodies” after vaccination showed a slight decrease in nicotine accumulation in the brain, as judged by the scans. However, another group of ten subjects, who showed “intermediate serum nicotine binding capacity and low affinity of antibodies” actually showed an increase in brain nicotine levels. What the PET scans showed was that “strong nicotine-antibody binding, which means high affinity, was associated with a decrease in brain nicotine accumulation. When binding was not strong, an increase in brain accumulation was observed.”
If the bond that holds the antibodies to the nicotine molecules is weak, the bond can break during passage through the blood-brain barrier, potentially allowing excess nicotine to flood in. This result, said Mukhin, tell us “we should care about not only the amount of antibody, but the quality of the antibody. We don’t want to have low-affinity antibodies because that can negate the anti-nicotine effects of the vaccination.”
Back to the drawing board? Not entirely. Another of the study authors, Yantao Zuo of Duke University Medical Center, said that “with reports of new generations of the vaccines showing potentially much higher potencies in animal studies, we are hopeful that our current findings and methodology in human research will facilitate understanding of how these work in smokers.”
Photo Credit:http://www.medgadget.com
Labels:
cigarettes,
nicotine,
smoking,
stop smoking,
vaccine
Subscribe to:
Posts (Atom)