The argument continues.
The argument continues.For more, see Marijuana Withdrawal.
See also Marijuana Withdrawal Revisited
Marijuana may not be a life-threatening drug, but is it an addictive one?
There is little evidence in animal models for tolerance and withdrawal, the classic determinants of addiction. For at least four decades, million of Americans have used marijuana without clear evidence of a withdrawal syndrome. Most recreational marijuana users find that too much pot in one day makes them lethargic and uncomfortable. Self-proclaimed marijuana addicts, on the other hand, report that pot energizes them, calms them down when they are nervous, or otherwise allows them to function normally. They feel lethargic and uncomfortable without it. Heavy marijuana users claim that tolerance does build. And when they withdraw from use, they report strong cravings.
Marijuana is the odd drug out. To the early researchers, it did not look like it should be addictive. Nevertheless, for some people, it is. Recently, a group of Italian researchers succeeded in demonstrating that THC releases dopamine along the reward pathway, like all other drugs of abuse. Some of the mystery of cannabis had been resolved by the end of the 1990s, after researchers had demonstrated that marijuana definitely increased dopamine activity in the ventral tegmental area. Some of the effects of pot are produced the old-fashioned way after all--through alterations along the limbic reward pathway.
By the year 2000, more than 100,000 Americans a year were seeking treatment for marijuana dependency, by some estimates.
A report prepared for Australia’s National Task Force on Cannabis put the matter straightforwardly:
There is good experimental evidence that chronic heavy cannabis users can develop tolerance to its subjective and cardiovascular effects, and there is suggestive evidence that some users may experience a withdrawal syndrome on the abrupt cessation of cannabis use. There is clinical and epidemiological evidence that some heavy cannabis users experience problems in controlling their cannabis use, and continue to use the drug despite experiencing adverse personal consequences of use. There is limited evidence in favour of a cannabis dependence syndrome analogous to the alcohol dependence syndrome. If the estimates of the community prevalence of drug dependence provided by the Epidemiologic Catchment Area Study are correct, then cannabis dependence is the most common form of dependence on illicit drugs.
While everyone was busy arguing over whether marijuana produced a classic withdrawal profile, a minority of users, commonly estimated at 10 per cent, found themselves unable to control their use of pot. Addiction to marijuana had been submerged in the welter of polyaddictions common to active addicts. The withdrawal rigors of, say, alcohol or heroin would drown out the subtler, more psychological manifestations of marijuana withdrawal.
What has emerged is a profile of marijuana withdrawal, where none existed before. The syndrome is marked by irritability, restlessness, generalized anxiety, hostility, depression, difficulty sleeping, excessive sweating, loose stools, loss of appetite, and a general “blah” feeling. Many patients complain of feeling like they have a low-grade flu, and they describe a psychological state of existential uncertainty—“inner unrest,” as one researcher calls it.
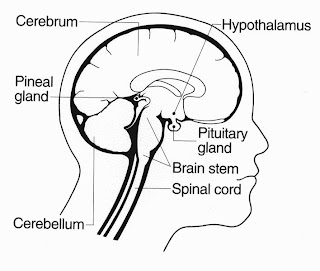
The most common marijuana withdrawal symptom is low-grade anxiety. Anxiety of this sort has a firm biochemical substrate, produced by withdrawal, craving, and detoxification from almost all drugs of abuse. It is not the kind of anxiety that can be deflected by forcibly thinking “happy thoughts,” or staying busy all the time. A peptide known as corticotrophin-releasing factor (CRF) is linked to this kind of anxiety.
Neurologists at the Scripps Research Institute in La Jolla, California, noting that anxiety is the universal keynote symptom of drug and alcohol withdrawal, started looking at the release of CRF in the amygdala. After documenting elevated CRF levels in rat brains during alcohol, heroin, and cocaine withdrawal, the researchers injected synthetic THC into 50 rats once a day for two weeks. (For better or worse, this is how many of the animal models simulate heavy, long-term pot use in humans). Then they gave the rats a THC agonist that bound to the THC receptors without activating them. The result: The rats exhibited withdrawal symptoms such as compulsive grooming and teeth chattering—the kinds of stress behaviors rats engage in when they are kicking the habit. In the end, when the scientists measured CRF levels in the amygdalas of the animals, they found three times as much CRF, compared to animal control groups.
While subtler and more drawn out, the process of kicking marijuana can now be demonstrated as a neurochemical fact. It appears that marijuana increases dopamine and serotonin levels through the intermediary activation of opiate and GABA receptors. Drugs like naloxone, which block heroin, might have a role to play in marijuana detoxification.
In the end, what surprised many observers was simply that the idea of treatment for marijuana dependence seemed to appeal to such a large number of people. The Addiction Research Foundation in Toronto has reported that even brief interventions, in the form of support group sessions, can be useful for addicted pot smokers.
--Excerpted from The Chemical Carousel: What Science Tells Us About Beating Addiction © Dirk Hanson 2008, 2009.