Monday, December 6, 2010
Cannabis and Severe Vomiting
For those of you who missed this, as I did, here is a belated account of a rare but altogether curious side effect of heavy marijuana use: cyclical vomiting.
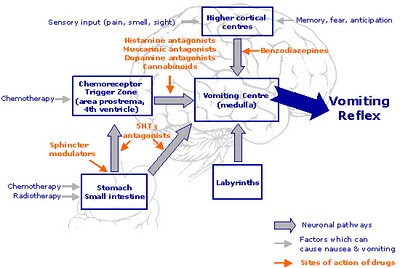
Nice, eh? And yes, it goes completely against the grain of what we think we know about marijuana: Ironically, cannabis is frequently employed to prevent the nausea and vomiting frequently associated with chemotherapy.
So what gives? The answer is that, so far, nobody really knows.
First things first: It appears to be a very rare side effect of regular marijuana use, and it was not documented in the medical literature until 2004. Given the long history of pot-smoking the world over, it is reasonable to ask where the cannabis emesis syndrome has been hiding all these years. A fair question, but one which, at this stage, has no satisfying answer.
Cannabinoid hyperemesis, as it's known, was first brought to wider attention earlier this year by the anonymous biomedical researcher who calls himself Drugmonkey. Posting on his eponymous blog, Drugmonkey documented cases of hyperemesis that had been reported in Australia and New Zealand, as well as Omaha and Boston in the U.S.
"There were two striking similarities across all these cases," Drugmonkey reported. "The first is that patients had discovered on their own that taking a hot bath or shower alleviated their symptoms. So afflicted individuals were taking multiple hot showers or baths per day to obtain symptom relief. The second similarity is, as you will have guessed, they were all cannabis users."
Heavy, regular cannabis users, most of them. And hot baths? Where did THAT come from?
More evidence was not long in coming. In February, researchers in the Division of Gastroenterology at William Beaumont Hospital in Royal Oak, Michigan, identified eight patients in their gastroenterology wards who were suffering from "otherwise unexplained refractory, recurrent vomiting." As the researchers reported in the journal Digestive Diseases and Sciences, there were two other significant features the eight patients shared: They were all chronic cannabis smokers--and they were all compulsive bathers.
The connection between uncontrolled vomiting and heavy toking seemed unequivocal: "Four out of five patients who discontinued cannabis use recovered from the syndrome," according to the published report, "while the other three patients who continued cannabis use, despite recommendations for cessation, continued to have this syndrome."
There is precious little anecdotal evidence to support this surprising finding. Occasionally, naive marijuana smokers will ingest too much and become sick to their stomach. And it is possible to incur the (brief) wrath of cyclic vomiting by eating way too many marijuana brownies, or other cannabis foodstuffs. Short of that, I am not familiar with vomiting as a documented side effect of regular cannabis use, and I venture to guess that most readers aren't, either.
However, the reports haven't stopped. This summer, an intriguing account appeared in Clinical Correlations, the official blog of New York University's Division of General Internal Medicine. Sarah A. Buckley and Nicholas M. Mark, 4th year medical students at the NYU School of Medicine, speculated on the cannabis hyperemesis phenomenon, and offered a formal definition: "A clinical syndrome characterized by intractable vomiting and abdominal pain associated with the unusual learned behavior of compulsive hot water bathing, occurring in the setting of long-term heavy marijuana use."
After reviewing 16 published papers on the syndrome, Buckley and Mark asked the obvious question: "How can marijuana, which is used in cancer clinics as an anti-emetic, cause intractable vomiting? And why would symptoms abate in response to high temperature?"
One possible mechanism involves marijuana's penchant for fats. Theoretically, this "lipophilicity" could cause increasingly toxic concentrations of THC over time, in susceptible people. "The abdominal pain and vomiting are explained by the effect of cannabinoids on CB-1 receptors in the intestinal nerve plexus," they write, "causing relaxation of the lower esophageal sphincter and inhibition of gastrointestinal motility." The authors speculate that low doses of THC might be anti-emetic, whereas in certain people, the high concentrations produced by long-term use could have the opposite effect.
As for the hot baths, Buckley and Mark note that "cannabis disrupts autonomic and thermoregulatory functions of the hippocampal-hypothalamic-pituitary system," which is loaded with CB-1 receptors. The researchers conclude, however, that the link between marijuana and thermoregulation "does not provide a causal relationship" for what they refer to as "this bizarre learned behavior."
These questions, like many questions having to do with regular marijuana use, are not likely to be answered definitively anytime soon, for a number of good reasons, some of which are delineated by the authors:
--"The legal status of marijuana makes eliciting an accurate drug history challenging."
--"The bizarre hot water bathing is likely often attributed to psychological conditions such as obsessive-compulsive behavior."
--"The knowledge of the anti-emetic effects of cannabis likely disguise cases of cannabinoid hyperemesis, leading to the erroneous belief that cannabis is treating cyclic vomiting rather than causing it."
--"The fact that this syndrome is so recently described and relatively unknown outside an esoteric subset of the GI [gastrointestinal] literature means that most clinicians are unaware of its existence."
Graphics Credit: http://www.oxygentimerelease.com/
Wednesday, December 1, 2010
MAPS Sponsors Psychedelic Confab
And J.R. will discuss his LSD trips with you.
The Multidisciplinary Association of Psychedelic Studies (MAPS) has put together a roster of very big psychedelic guns, as well as a few surprises, for its mini-conference on December 12-13 in Los Angeles. On tap for the convocation are such luminaries as Stanislav Grof of Holotropic Breathwork fame; as well as Charles Grob, professor of Psychiatry and Pediatrics at the UCLA School of Medicine and a psychedelic research of long standing who recently studied the effects of psilocybin on death anxiety in terminal cancer patients.
“Catalysts: The Impact of Psychedelics from Consciousness to the Clinic, and from Culture to Creativity” will feature presentations and discussions on “psychedelic science, the current state of psychedelic research, and clinical applications for therapeutic use.”
Other experts among the scientists, physicians, psychologists, writers, and artists expected to attend include Rick Doblin, the founder of MAPS, who has specialized in research on MDMA (Ecstasy) as a treatment for posttraumatic stress disorder. Another scheduled attendee, James Fadiman, was introduced to the field of psychedelic drugs by his Harvard undergraduate advisor Richard Alpert, who later became well known as Baba Ram Dass. Fadiman holds the distinction of being the last LSD researcher to be shut down by the U.S. government, when he was at San Francisco State University in 1972.
Also in attendance will be Julie Holland, an assistant professor of psychiatry at NYU School of Medicine, and the author of “Ecstasy: A Complete Guide,” and Clare Wilkins, director of the Pangea Biomedics Ibogaine Clinic in Mexico.
Special Bonus Appearance:
I can’t imagine that anyone under the age of 55 is likely to know who Larry Hagman is. Long ago, he was on a camp TV show about a Texas oil bazillionaire with nasty habits. Not only was he a big TV star, he was also old enough to have been around when LSD psychotherapy came to the couches of Hollywood analysts for a brief period in the 1960s and attracted some other odd ducks like Cary Grant and James Coburn. Hagman, Star of TV’s “Dallas” and “I Dream of Jeannie,” will discuss his experiences with LSD psychotherapy.
Earlier, he talked about his experiences in a 2003 interview with Rick Doblin, published in the MAPS journal and excerpted below:
Before I tried LSD, I'd been going to a psychologist for a couple of years…. I had been addicted to tobacco and Bontril, a mild form of amphetamine, doctor-prescribed of course….
I was backstage at a performance one time with Crosby, Stills & Nash and I was talking about it to David Crosby. David said, well, shit, man, here. He handed me a handful of little pills. I said what the fuck? He says this is LSD. It was the best going around at that time. This was before Blue Cheer and Windowpane. This was the original Owsley. He gave me about 25 pills. I said, well, how much should I take? He says, well, don't take more than one….
… my first acid trip was the most illuminating experience of my life. I would highly recommend it for people who study and prepare for it and who are not neurotic or psychotic. I don't know what it would do to psychotic people. I know what it does to neurotic people who can't handle that. They get terrified and do crazy things like jumping out of windows and stuff like that. That's happened to a couple of friends of mine.
Graphics Credit: http://en.wikipedia.org/wiki/Larry_Hagman
World AIDS Day
Testing, Testing.
Guest Post By Kevin Fenton, M.D., Ph.D., FFPH, Director, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention (CDC).
Every year on December 1, we commemorate World AIDS Day to bring attention to the tremendous impact of the HIV epidemic in the United States and around the world. In observance of World AIDS Day, today CDC launched a special report, CDC Vital Signs on HIV Testing in the United States, in recognition of the pivotal role that HIV testing plays in our national HIV prevention strategy.
Some highlights of the CDC Vital Signs report on HIV testing include:
• In 2009, an estimated 82.9 million Americans ages 18-64—45% of this age group—reported they had been tested for HIV.
• At least 1 in 3 Americans who test positive for HIV is tested too late in his or her infection to get the full advantage of life-saving treatment.
• Gay, bisexual, or other men who have sex with men have the highest rates of HIV, but a 2008 study conducted in 21 major US cities, found that about 40% had not been tested in the past year.
• African Americans made up more than half of HIV diagnoses in 2008, but 2 in 5 African Americans have never been tested.
CDC recommended in 2006 that HIV testing become a routine part of medical care, including testing of all adolescents and adults at least once, testing at least annually for persons at increased risk, and testing of women during each pregnancy. Since that time, HIV testing has increased, and more people are being tested for HIV than ever before. However, many challenges remain: 55% of Americans ages 18 to 64 still have never been tested, according to CDC Vital Signs. And of the estimated 1.1 million people living with HIV in the United States, 1 in 5 do not know they are infected.
More needs to be done. HIV testing is vitally important because it can save lives. For anyone who is infected, it is important to know his or her HIV status in order to access effective life-extending treatment, avoid HIV transmission to partners, and have a better quality of life.
Treatment for HIV is most effective before symptoms develop. It can do much to slow the infection that leads to AIDS and death. Without treatment a person infected with HIV will develop AIDS in about 10 years. With early treatment a 25-year-old adult can survive on average 39 more years.
According to the Vital Signs report, nearly one-third (32%) of the people found with HIV in 2007 were diagnosed late. This means that they likely had HIV for a long time without knowing it because they developed AIDS soon (less than one year) after their HIV test.
Health care providers play a critical role in stopping the spread of HIV as most HIV testing is conducted in health care settings. It is important that patients listen to their doctors and it is important that doctors and other health care providers speak openly and honestly with patients about HIV, and offer routine testing per CDC recommendations.
CDC also plays a critical role. We are committed to strengthening our efforts against the epidemic and working with partners to increase HIV testing. CDC continues to expand its efforts in areas where the burden of disease is greatest. We recently announced an expansion of a successful HIV testing initiative to reach more hard-hit populations, including African Americans, Latinos, men who have sex with men and injection drug users. In 2010, CDC provided more than $60 million to support HIV testing efforts in 30 of the hardest hit jurisdictions in the United States.
In addition, CDC provides funds to all health departments and more than 130 community-based organizations to implement HIV prevention programs, including HIV testing. We are also working to get messages out about testing through the Act Against AIDS campaign. Of critical importance, the National HIV/AIDS Strategy, recently released by the White House, provides a new opportunity to refocus and intensify federal, state, and local HIV testing efforts.
Now more than ever, effective HIV prevention is a critical public health priority for the U.S. and the world, and HIV testing to identify those infected is a vital component of that effort. Working together, we can increase HIV testing. Everyone needs to know how important HIV testing is – it is a simple measure that can literally save the health and lives of hundreds of thousands of Americans and help to bring an end to this tragic epidemic.
Monday, November 29, 2010
Challenging the Received Wisdom on Tobacco Addiction
What does it take to get hooked on nicotine?
--Smokers who smoke five or fewer cigarettes per day can still become addicted to tobacco.
--Tobacco addiction can also be present in non-daily smokers.
--Nicotine withdrawal symptoms do not necessarily begin within 24 hours.
These and other controversial assertions come from Joseph R DiFranza, a physician with the Department of Family Medicine and Community Health at the University of Massachusetts Medical School. Dr. DiFranza recently authored a provocative examination of smoking truisms in an article for the online publication Harm Reduction Journal.
In an attack on what he calls the Threshold Model of Addiction, DiFranza defines the model as follows:
In brief, the threshold model maintains that until tobacco consumption is maintained above a threshold of 5-10 cigarettes per day (cpd) for a prolonged period, smokers are free of all symptoms of tobacco addiction. It holds that declining blood nicotine levels trigger withdrawal symptoms so quickly that addicted smokers must protect their nicotine levels by smoking at least 5 cpd. The threshold model states that until addiction is established with moderate daily smoking, smoking is motivated and maintained by peer pressure, pleasure seeking and the social rewards of smoking.
DiFranza breaks this prevailing paradigm into a half-dozen hypotheses, offering his opinion on the state of scientific evidence that, in his view, refutes every one of them:
--Hypothesis 1. Tobacco addiction cannot occur in nondaily smokers, or even in daily smokers who regularly consume fewer than 5 cpd.
DiFranza’s response: “Although it is difficult to prove a negative, this hypothesis would be supported if study after study demonstrated that all surveyed subthreshold smokers (individuals who smoke < 5 cpd) have no symptoms of addiction…. Since no studies have demonstrated a complete lack of addiction symptoms in any representative population of subthreshold smokers, the peer reviewed literature soundly refutes the hypothesis that tobacco addiction requires as a prerequisite the daily consumption of 5-10 cigarettes. The threshold model and the DSM are wrong. “
--Hypothesis 2. Tobacco addiction requires prolonged daily use as a prerequisite.
Response: “Many subjects developed symptoms quite soon after the onset of intermittent tobacco use. These findings have been replicated in several longitudinal studies, in cross-sectional studies showing symptoms of addiction in nondaily smokers, and by case histories showing the same.”
Hypothesis 3. Nicotine withdrawal symptoms begin within 24 hours in all smokers.
“The standard subject in all early smoking studies was an adult who had been a heavy daily smoker for decades. Such individuals do experience nicotine withdrawal soon after their last cigarette. A problem arises when this observation is inappropriately generalized by applying it to all smokers, including children, novices and nondaily smokers.”
Hypothesis 4. Addicted smokers must maintain nicotine above a threshold blood concentration to avoid withdrawal.
“Since a person must smoke at least 5 cpd to maintain a minimum nicotine level throughout the day, another approach to testing this hypothesis would be to determine if all smokers that experience withdrawal symptoms smoke at least 5 cpd. This test has been completed over a dozen times, and always with the same result. Withdrawal symptoms have been reported in smokers of fewer than 5 cpd in every study that has examined this issue.”
Hypothesis 5. Psychosocial factors maintain smoking over the several years it may take to reach threshold levels of smoking.
“There must be thousands of studies that demonstrate that social factors such as socioeconomic status, smoking by family and friends, cigarette advertising, the availability of cigarettes, smoking depictions in movies, and attitudes and beliefs are predictive of which youth will try smoking. However, if such factors sustain tobacco use until tobacco addiction develops, they should predict which smokers will advance to addiction in prospective studies. But this has not been shown. None of more than 40 psychosocial risk factors for the onset of smoking was able to predict the progression to tobacco addiction. The author is aware of no studies that establish that peer pressure of other social factors sustain adolescent or young adult smoking over the 4 or 5 years it may take for smokers to reach threshold levels of smoking. “
Hypothesis 6. Increasing tolerance to the pleasurable effects of smoking drives the escalation in tobacco use up to the threshold of addiction.
“The author is not aware of any studies that demonstrate that smokers must smoke more cigarettes over time to obtain the same amount of pleasure (for example smoking 10 cpd to obtain the same pleasure initially obtained from smoking 1 cpd. Indeed, our data indicate that the pleasure obtained from smoking each cigarette actually increases in proportion to the degree of addiction, with pleasure ratings correlating strongly with addiction severity. While this is only one study, it directly contradicts the hypothesis that non-addicted novice smokers obtain much more pleasure from each cigarette than do addicted heavy smokers.”
Photo Credit: http://nikotin.floridadmat.com/
Wednesday, November 24, 2010
DEA Slaps Temporary Ban on Spice and Other “Fake Pot” Products
Synthetic cannabis now illegal for one year.
The material below is excerpted directly from the official press release of the U.S Drug Enforcement Administration Public Affairs Office:
The United States Drug Enforcement Administration (DEA) is using its emergency scheduling authority to temporarily control five chemicals (JWH-018, JWH-073, JWH-200, CP-47,497, and cannabicyclohexanol) used to make “fake pot” products. Except as authorized by law, this action will make possessing and selling these chemicals or the products that contain them illegal in the U.S. for at least one year while the DEA and the United States Department of Health and Human Services (DHHS) further study whether these chemicals and products should be permanently controlled.
A Notice of Intent to Temporarily Control was published in the Federal Register today to alert the public to this action. After no fewer than 30 days, DEA will publish in the Federal Register a Final Rule to Temporarily Control these chemicals for at least 12 months with the possibility of a six-month extension. They will be designated as Schedule I substances, the most restrictive category, which is reserved for unsafe, highly abused substances with no medical usage.
Over the past year, smokable herbal blends marketed as being “legal” and providing a marijuana-like high, have become increasingly popular, particularly among teens and young adults. These products consist of plant material that has been coated with research chemicals that mimic THC, the active ingredient in marijuana, and are sold at a variety of retail outlets, in head shops and over the Internet. These chemicals, however, have not been approved by the FDA for human consumption and there is no oversight of the manufacturing process. Brands such as “Spice,” “K2,” “Blaze,” and “Red X Dawn” are labeled as incense to mask their intended purpose.
Graphics Credit: http://thefreshscent.com/
Labels:
DEA,
designer drugs,
k2,
spice,
synthetic cannabis,
synthetic marijuana
Monday, November 22, 2010
Drug-Drug Interactions to Watch Out For
P450 enzymes and “poor metabolizers.”
The finding, published in Science,
So what? Well, for starters, “cytochrome P450 enzymes are responsible for the phase I metabolism of approximately 75% of known pharmaceuticals,” write Jonathan Rittle and Michael T. Green at Pennsylvania State University’s Department of Chemistry. And in fact, only six of the more than 50 enzymes in the P450 family account for 90% of drug metabolization in humans--the compound known as CYP2D6 being the most crucial.
In a Penn State press release, lead author Michael Green, an associate professor of chemistry, noted that human populations vary widely in the version of genes they carry for P450 enzymes. According to Green, “adverse drug-drug interactions are a well-known problem…. Now that we can see those state changes on a molecular level, a deeper investigation is possible.”
The wide variation in enzymatic reactions, says Green, causes very real consequences. People with two copies of variant alleles are poor metabolizers, people with two copies of the standard genetic variety are normal metabolizers, whereas people with one of each are “reduced” metabolizers. (People who inherit multiple copies of the alleles become “ultrarapid” metabolizers.)
“With a drug such as caffeine, for example, one population of people might be fast metabolizers, while another might metabolize the drug more slowly,” Green said. "Because the risk of caffeine-induced heart attack may be higher in slow metabolizers, the ability to actually take a snapshot of the phase changes of the P450 enzymes could help us to understand better how certain chemicals can affect people in vastly different ways."
There are dozens of specific cases like the caffeine example. Moreover, the genetic situation is complicated by other factors. Writing in American Family Physician, Tom Lynch and Amy Price explain that cytochrome P450 enzymes “can be inhibited or induced by drugs, resulting in clinically significant drug-drug interactions that can cause unanticipated adverse reactions or therapeutic failures. Interactions with warfarin, antidepressants, antiepileptic drugs, and statins often involve the cytochrome P450 enzymes.” Testing for these interactions is expensive, and “it has not been determined if routine use of these tests will improve outcomes.”
Not a pretty picture. And just to further complicate matters, some drugs can induce or inhibit CYP450 enzymes differentially, depending upon the dosage. “For instance,” write Lynch and Price, “sertraline (Zoloft) is considered a mild inhibitor of CYP2D6 at a dose of 50 mg, but if the dose is increased to 200 mg, it becomes a potent inhibitor. Inhibitory effects usually occur immediately.” Also, drugs can be metabolized by, and at the same time serve to inhibit, the enzyme in question, as in the case of erythromycin.
So it is buyer beware, and listen to your body’s feedback when embarking on a course of new drugs. Recommended dosages are just that: recommendations. If you feel that the drug in question is doing too much or too little, ask your prescribing doctor about drug-drug interactions and about fast and slow drug metabolizers. Of course, they should be telling YOU about that, but.
Some known enzymatic drug interactions to bear in mind:
Drugs that potentially inhibit P450 enzymes—Tagamet, Cipro, Luvox, Prozac, Flagyl, Benadryl, Paxil, Lamisil, and grapefruit juice.
Drugs that potentially increase the activity of P450 enzymes—Tegretol, phenobarbital, tobacco, Dilantin, rifampin, St. John’s wort.
------
Adverse drug-drug interactions involving P450 enzymes:
Amiodarone (Cordarone) combined with Warfarin (Coumadin): possible bleeding due to increased warfarin activity.
Tegretol, phenobarbital, and Dilantin combined with contraceptives containing ethinyl estradiol: possible unplanned pregnancies due to reduced contraceptive activity.
Clarithromycin, erythromycin, and telithromycin combined with Zocor: possible muscle disorders due to increased Zocor levels.
Prozac combined with Risperidone (Risperdal): increased risk of adverse effects from the antipsychotic drug risperidone.
Grapefruit juice combined with Buspirone (Buspar): Dizziness and other effects of “serotonin syndrome” due to increased buspirone activity.
Rittle, J., & Green, M. (2010). Cytochrome P450 Compound I: Capture, Characterization, and C-H Bond Activation Kinetics Science, 330 (6006), 933-937 DOI: 10.1126/science.1193478
Graphics Credit: http://elcamino.dnadirect.com/
Thursday, November 18, 2010
The Day After
How’s that no-smoking pledge going?
This post is not meant for most of you. Those of you who never smoked, or smoked and quit successfully—move along, maybe check out my earlier posts about smoking this month.
But for those of you who have decided to take the 35th annual Great American Smokeout seriously—for those of you who decided today, or yesterday, or recently, to quit smoking—I have a few remarks, if you have a moment. I’m fairly trustworthy on this subject. I’m a science writer, I follow the field of addiction science, and I smoked a pack of Camel filters a day for about 25 years. In addition, I quit smoking using the most recently available smoking cessation aids—nicotine patches and anti-craving medication, in this case Zyban, a.k.a. Wellbutrin.
I had decided, after the usual smoker’s run of unsuccessful independent quitting attempts, that the only real hope I had for success was to throw myself into the hands of my primary care physician. Happily, Dr. Joe is a young example of the last of the breed, a lingering remnant of a tribe that used to be known as family doctors. When I told Dr. Joe of my plans to quit smoking, he was overjoyed. Too overjoyed, it seemed to me. As it turned out, there were grounds for my suspicion. Dr. Joe had recently returned from a smoking cessation seminar at the Mayo Clinic in Rochester, Minnesota, with a grab bag of refinements and alternative approaches for setting up a no-smoking regimen. Furthermore, he made it clear that, if necessary—if I forced him to it through relentless noncompliance—he was fully prepared to order regular blood workups to detect and quantify my nicotine levels.
Of course, I instantly regretted setting a foot into this ring, but once Dr. Joe started flinging prescriptions for patches and pills my way, I realized I was in it up to my wallet (Insurance companies weren’t paying for nicotine cessation products, ever, at that time).
Most smokers know the current drill. A few weeks with nicotine patches or gum or nasal spray, combined with a short course of Zyban or Chantix to further reduce cravings, and then you are expected to fly out of the nest and spread the good news. Most smokers know that even this controversial armamentarium is not going to completely spare them from a rare and special kind of suffering: addictive craving for nicotine. It’s a mean, rough ride, as everyone knows.
But if you take a few of the major potholes out of the road, smooth over the really big bumps just a little, fill in the low spots a bit as well, you have a fighting chance—especially if you have tried and failed before (almost nobody pulls it off on the first attempt).
Here are the key features of the program, as my doctor worked it up for me:
--Stronger patches. Mayo Clinic and other institutions had made an important discovery, my doctor said. People weren’t wearing strong enough patches. There was a system of matching up patch strength to amount and duration of smoking, and then a step-down procedure, to less and less powerful patches, and it was all listed on the packages, but because of great nervousness over medical complications by a very few individuals who overdid the patch and then chain-smoked on top of that, the result was that the patches as marketed weren’t strong enough, many doctors felt. The advice was to start strong, with the strongest patch available (and perhaps there was even a patient or two who doubled up, ahem).
--Longer patches. Start strong—and go long. The whole nicotine replacement plan is supposed to last a month or two. Phooey, said Dr. Joe. No telling in advance how long the process will take. There is no set timetable. How long would I be wearing patches and tapering the dose? As long as it took, Dr. Joe inferred, for me not to need them anymore. He seemed prepared to keep me on patches the rest of my life, if it kept me from picking up a cigarette. In the end, when I took off my final, tiny patch, I had been using them for a little less than six months. The recommended five-star treatment plan in the literature and on the packages calls for only 10 weeks, tops.
--Pharmaceuticals. It is admittedly hard to separate out placebo effects from drug effects, in the case of something as elusive as cigarette urges. But I do believe that Zyban took the edge off the worst of my cigarette cravings. It did not eliminate them, anymore than the patches eliminated them. But the medication effectively dissipated the grip of that moment of panic, when you have risen from your chair and set about finding your coat and car keys for a run to the gas station to buy a pack of cigarettes. Or at least that’s the way it felt to me.
--Exercise. Trite? You bet, and you can be sure that I winced and offered a tired smile when I heard my doctor bore in on the subject. Since I knew him to be a crazed bicyclist, I was prepared to disregard most of what he had to say. But his insistence sent me back to the research literature on exercise and its effect on dopamine, serotonin, acetylcholine, and endorphin levels. So I took him up on that firm suggestion as well, and found that, at the least, it helped with a period of rocky sleep in the beginning.
--Diet. No huge changes, just watching the sweets in an effort to avoid surging blood sugar levels. Fruit helps, since constipation is a common side effect of nicotine cessation—just the opposite of how it works with heroin. I continued to drink coffee, but for a while it didn’t taste as good.
--Relaxation. Quitting smoking makes you tense. You think I’m being funny? Quitting smoking makes you tense all over, mentally and physically. During the first few days you’ll notice that your body is clenched, held rigidly. Your posture is likely to be anything but relaxed; your physical movements can be jerky and awkward. A few minutes a day spent sitting with eyes closed, in a relaxed upright posture, thinking of nothing or concentrating on your breathing or meditating either formally or casually, can bring partial relief from all that tension. And on some days, that can be crucial.
--Determination. Unfortunately, it wasn’t until everyone around me—my wife, children, parents, close friends, work associates—had all, I sensed, basically given up on me, silently condemning me to the category of Lifetime Smoker, that I finally managed to make a successful run at a major life problem. There are better ways to work up your determination. Find and employ them.
With time, an involved partner, nicotine replacement, and the right medication, the deal can be done. There has never been a better time in history to be a smoker who has decided to quit.
Graphics Credit: http://adoholik.com/
Subscribe to:
Posts (Atom)