Showing posts with label marijuana withdrawal. Show all posts
Showing posts with label marijuana withdrawal. Show all posts
Monday, February 1, 2016
A Roundtable Discussion on Cannabis Use Disorder
Addressing the habit-forming aspects of marijuana.
A trio of leading marijuana scientists participated in a panel discussion moderated by Dr. Daniele Piomelli from the School of Medicine at the University of California-Irvine, and published in a recent issue of the journal Cannabis and Cannabinoid Research.
Dr. Margaret Haney is with the New York State Psychiatric Institute at Columbia University Medical Center; Dr. Alan J. Budney is affiliated with the Geisel School of Medicine at Dartmouth College; and Dr. Pier Vincenzo Piazza works at the Magendie Neurocenter in Bordeaux, France.
Excerpts from the long discussion appear below:
It seems that most specialists in the field agree that Cannabis is addictive. If you had to choose one piece of evidence, either clinical evidence or animal experiment evidence, in support of this conclusion, which one would you pick?
Dr. Margaret Haney: “One of the key features for me is demonstrating that there is a pharmacologically specific withdrawal from Cannabis use…. We can demonstrate that daily smokers go through a time-dependent and pharmacologically specific withdrawal when they abstain from Cannabis…. I think another really important feature is the clinical data showing how high relapse rates are with Cannabis. Although Cannabis may have a lower abuse liability than other drugs like cocaine or nicotine, once somebody has developed a dependence on the drug, then quitting becomes extremely difficult.
Dr. Alan J. Budney: “If I had to pick out the ‘smoking gun’ to convince the public and the scientific world that Cannabis Use Disorder (CUD) is real, then it would be the data from clinical epidemiological research…. the data on CUDs are remarkably similar to the other substance use disorders…. for a substantial number of people, Cannabis use causes similar and substantial problems that are comparable to other types of drugs that we all agree have addictive potential.”
Dr. Pier Vincenzo Piazza: “[In] Australia, Canada, the United States, and the European Union, over the last two years Cannabis represents the highest new entries for treatment in specialized centers…. Since these four countries have very different rates of referral of patients by the judicial system, these figures really mean that patients experience a discomfort high enough to spontaneously seek treatment…. In France, for example, as well as in many other European countries, referral from the judicial system is very low. Nevertheless, the demand for treatment for CUD is now the highest of all drugs, legal and illegal.”
What is curious is that we now accept the concept that Cannabis is addictive, but for many years we have been told that it was not. Why is it that, for so long, the scientific community failed to recognize the addictive properties of Cannabis?
Dr. Margaret Haney: “I have been speaking about Cannabis addiction for 20 years and was met by full-on boredom for the first 15 years because I felt that scientists, like the public at large, just viewed Cannabis as a benign compound not too different from caffeine in a way…. THC is lipophilic, and so long-lasting, withdrawal takes quite a while to manifest…. if an individual is dependent on nicotine, he or she cannot go a couple of hours without experiencing withdrawal. A heavy Cannabis user, by contrast, has to go quite a while before experiencing withdrawal, and so it was not quite as obvious to people that withdrawal existed.”
Dr. Alan J. Budney: “Moreover, many of those that have experience with using Cannabis, do not get addicted, develop problems, or experience withdrawal. Although the same is true for those who have used alcohol or even opiates, for reasons that are not completely clear, the personal experience of those who used Cannabis and did not develop problems or experience withdrawal, seems to lead to the perception that Cannabis is not a substance that others can become addicted to.”
Dr. Pier Vincenzo Piazza: “What we know now is that, since cannabidiol is an antagonist of THC, the greater the ratio between THC and cannabidiol the greater the risk for Cannabis to be addictive…. Now, we are up to a 5- to 10-fold difference in favor of THC, making Cannabis more addictive.”
How addictive is Cannabis? Is it more addictive than, say, tobacco or alcohol? Is it less addictive? Is this question even correctly asked? Is there a better way to ask it?
Dr. Alan J. Budney: [I] would like to emphasize a point so that our audience does not think we are going way overboard and engaging in reefer madness related to the severity of Cannabis addiction. All factors held constant, the pharmacology of opiates would probably produce a more severe addiction…. Access, dose, route of administration, societal acceptance, perceived risk, cost, societal consequences for use or intoxication, and multiple other factors contribute to the real-world question of how addictive a drug is compared to another.”
Dr. Margaret Haney: “My opinion is that Cannabis has a lower abuse liability than something like cocaine [but] even if Cannabis has a lower abuse liability, the sheer number of people using it will result in a large number of people with a use disorder….”
Dr. Pier Vincenzo Piazza: “If we try to express abuse liability in numbers, the abuse liability for Cannabis… is between 10% and 15%, depending on the survey you look at. However, I believe that abuse liability should also be measured by a second factor; that is, how easy it is to quit if you have developed a substance use disorder. My understanding… is that stopping Cannabis use, if you have developed CUD, is not easier than other drugs.”
The major point, all three experts agree, is that marijuana cannot be considered a completely benign drug. “Cannabis is not the worst drug,” says Dr. Haney, “but it is not a drug without consequences. Again, societal attitudes often seem to skew one way or the other; it is all good or it is all bad, when it is clearly both.”
Graphics Credit: hhttp://moodsurfing.com
Sunday, June 15, 2014
NIDA’s Dark View of Teen Marijuana Use
Federal study also discusses medical marijuana.
Considering the impasse on marijuana policy between state and federal governments in the U.S., the primary government agency in charge of drug research—NIDA, the National Institute on Drug Abuse—would seem to be caught between a rock and a hard place. Neuroscientists and other marijuana investigators who do research under NIDA grants have a fine line to walk in their efforts to disseminate research findings on cannabis.
From a public health point of view, NIDA is expected to keep up the pressure against drug legalization, or at least keep out of the fight, while also researching the medical pros and cons of cannabis. So it was with some interest that drug policy officials took in a recent article in the New England Journal of Medicine by NIDA director Nora Volkow titled “Adverse Health Effects of Marijuana Use.”
While the press has understandably centered on the risk of marijuana use among teens, which is the focus of the study, the report also contains some surprising admissions about marijuana’s health benefits as well as its addictive potential.
The teen risk emphasis comes from recent studies on two fronts—impaired driving and impaired brain function. The first is seriously confounded by dual use with alcohol, and the second is based, at least in part, on a controversial long-term study showing that marijuana use in the early years demonstrably lowers adult IQs.
No one would suggest that heavy marijuana smoking is good for developing teen brains, and there is sufficient evidence to worry about impairment to memory and to certain so-called “executive” cognitive functions. It is not clear how lasting these effects can be, but lead author Volkow is confident enough to say in a prepared statement that “Physicians in particular can play a role in conveying to families that early marijuana use can interfere with crucial social and developmental milestones and can impair cognitive development.”
That these negative effects can be the outcome of heavy pot smoking in the teen years seems established beyond reasonable doubt. The extent and duration of these negative outcomes remain the topic of vociferous debate—although it is increasingly clear that the body’s endogenous cannabinoid system plays a key role in synapse formation during early brain development.
Meanwhile, the report re-emphasized the fact that marijuana is an addictive drug for some users—a fact that should not need re-emphasizing, but, lamentably, does. As Volkow and her co-authors write: “The evidence clearly indicates that long-term marijuana use can lead to addiction. Indeed, approximately 9% of those who experiment with marijuana will become addicted.”
Moreover, as regular readers of Addiction Inbox already know, “there is also recognition of a bona fide cannabis withdrawal syndrome (with symptoms that include irritability, sleeping difficulties, dysphoria, craving, and anxiety), which makes cessation difficult and contributes to relapse.” And, in line with the report’s overall theme, “those who begin in adolescence are approximately 2 to 4 times as likely to have symptoms of cannabis dependence within 2 years after first use.”
To their credit, the investigators decline to endorse the claim that marijuana use exacerbates or initiates episodes of illness in patients with schizophrenia and other psychoses, noting that “it is inherently difficult to establish causality in these types of studies because factors other than marijuana use may be directly associated with the risk of mental illness.” Furthermore, while early marijuana use is associated with an increased risk of dropping out of school, “reports of shared environmental factors that influence the risks of using cannabis at a young age and dropping out of school suggest that the relationship may be more complex…. The relationship between cannabis use by young people and psychosocial harm is likely to be multifaceted, which may explain the inconsistencies among studies.”
Indeed. The report also declares that the effects of long-term pot smoking on the risk of lung cancer are “unclear,” and that “the smoking of cigarettes containing both marijuana and tobacco products is a potential confounding factor with a prevalence that varies dramatically among countries.”
In conclusion, the strict demands of causality mean that the long-term effect of chronic marijuana exposure is not known with any certainty. It is possible, even likely, that these effects can vary dramatically from one smoker to another. But the equally persuasive demands of common sense dictate that inhaling dried, super-heated vegetable matter on a regular basis is likely to degrade your health, the more so if you are young and healthy to begin with.
As for other health issues: “The authoritative report by the Institute of Medicine, Marijuana and Medicine, acknowledges the potential benefits of smoking marijuana in stimulating appetite, particularly in patients with the acquired immunodeficiency syndrome (AIDS) and the related wasting syndrome, and in combating chemotherapy-induced nausea and vomiting, severe pain, and some forms of spasticity. The report also indicates that there is some evidence for the benefit of using marijuana to decrease intraocular pressure in the treatment of glaucoma.”
A detailed section titled “Clinical Conditions with Symptoms That May Be Relieved by Treatment with Marijuana or other Cannabinoids” brought additional research to light:
—Glaucoma: “More research is needed to establish whether molecules that modulate the endocannabinoid system may not only reduce intraocular pressure but also provide a neuroprotective benefit in patients with glaucoma.”
—Nausea: “THC is an effective antiemetic agent in patients undergoing chemotherapy, but patients often state that marijuana is more effective in suppressing nausea…. Paradoxically, increased vomiting (hyperemesis) has been reported with repeated marijuana use. [See various blog posts by Drugmonkey and me, starting with this and this.]
—AIDS-associated conditions: “Smoked or ingested cannabis improves appetite and leads to weight gain and improved mood and quality of life among patients with AIDS.”
—Chronic pain: “Studies have shown that cannabinoids acting through central CB1 receptors, and possibly peripheral CB1 and CB2 receptors, play important roles in… various models of pain. These findings are consistent with reports that marijuana may be effective in ameliorating neuropathic pain, even at very low levels of THC.”
—Inflammation: “Cannabinoids (e.g., THC and cannabidiol) have substantial anti-inflammatory effects…. Animal models have shown that cannabidiol is a promising candidate for the treatment of rheumatoid arthritis and for inflammatory diseases of the gastrointestinal tract (e.g., ulcerative colitis and Crohn’s disease).”
—Multiple sclerosis: “Nabiximols (Sativex, GW Pharmaceuticals), an oromucosal spray that delivers a mix of THC and cannabidiol, appears to be an effective treatment for neuropathic pain, disturbed sleep, and spasticity in patients with multiple sclerosis. Sativex… is currently being reviewed in phase 3 trials in the United States in order to gain approval from the Food and Drug Administration.”
—Epilepsy: In a recent small survey of parents who use marijuana with a high cannabidiol content to treat epileptic seizures in their children, 11% reported completed freedom from seizures…. Although such reports are promising, insufficient safety and efficacy data are available on the use of cannabis botanical for the treatment of epilepsy. However, there is increasing evidence of the role of cannabidiol as an antiepileptic agent in animal models.”
Volkow N.D., Baler R.D., Compton W.M. & Weiss S.R.B. Adverse health effects of marijuana use., The New England journal of medicine, PMID: 24897085
Wednesday, March 20, 2013
Drug News in Brief
Short takes on matters various.
Taking Aim at Pot—Researchers have recently made clinical efforts to test three drugs that might help during marijuana withdrawal to keep pot abstainers on the straight and narrow. Researchers at Columbia University, led by Margaret Haney, have been testing a synthetic THC compound called nabilone. The drug is designed to address sleep and appetite problems during withdrawal. Whether it is any better tolerated by users than Marinol, Uncle Sam’s widely unpopular version of synthetic THC, remains to be seen. This approach can be viewed rather like methadone or buprenorphine substitution therapy. Meanwhile, work goes on with lofexidine, a drug sometimes used in combination with naltrexone for opiate detoxification. A 2008 study in Psychopharmacology showed a modest improvement over placebo when lofexidine was used for marijuana abstinence, but it worked much better when combined with, yes, synthetic THC. Finally, velafaxine, better known as the antidepressant Effexor, was used in a randomized, double-blind, placebo controlled trial of marijuana-dependent outpatients recently published in Addiction. Not only did velafaxine fail to help the patients with their cannabis dependence, but in fact “may lead to an increase in cannabis use.”
Smoking is Bad to the Bone—The Journal of Adolescent Health reports that cigarette smoking dramatically impacts the rate of bone density growth in teenage girls. Young women may be smoking their way toward a future of osteoporosis, the loss of bone density that often plagues older women. “This age group is when you should gain about 50 percent of your bone accrual,” reports study author Lorah Dorn at Cincinnati Children’s Hospital Medical Center, in Science News. A 2001 study of adult smokers found that smoking increased the risk of hip fracture by 31% in women. In addition, at the recent annual meeting of the American Academy of Orthopedic Surgeons, researchers reported on a study of 6,779 patients undergoing treatment for spinal disorders with severe pain. Those who quit smoking during treatment reported greater pain improvement than patients who didn't stop smoking.
Dr. Google Will See You Now—Researchers are starting to data-mine the Internet to identify unanticipated side effects and interactions between prescription drugs. According to an article in Science by Sean Treacy, one study in 2011 data-mined reports to the FDA from doctors, nurses, and patients, and “uncovered a hidden drug interaction: When taken together the antidepressant paroxetine and the cholesterol suppressant pravastatin can cause hyperglycemia, or high blood sugar.” Bioinformatics researcher Nigam Shah of Stanford told the magazine that “if a lot of people are concerned about a symptom, that in itself is valuable information.”
Fetal Health—Scientists have traced out a molecular signaling pathway that appears to play a crucial role in the development of fetal alcohol spectrum disorders (FASD). According to the researchers, whose study was published in the Proceedings of the National Academy of Sciences, “ethanol may cause FASD in part by decreasing the adhesion of the developmentally critical L1 cell adhesion molecule through interactions with an alcohol binding pocket on the extracellular domain.” In English, it means that the research points to strong candidate genes, therefore identifying a specific locus of action for future drugs designed to block alcohol neurotoxicity in the womb. A group led by Michael Charness at Harvard Medical School did the work, building on previous studies that identified the alcohol sensitivity of L1 adhesion molecules. “Prenatal alcohol exposure is the leading preventable cause of birth defects and developmental disorders in the United States,” according to perennial Acting NIAAA Director Kenneth Warren, in an NIH news release.
Photo Credit: http://jimbaker.wordpress.com/
Thursday, December 27, 2012
The Year in Drugs
 Top Posts at Addiction Inbox.
Top Posts at Addiction Inbox.By the look of it, readers had marijuana on their minds in 2012. Of the posts at Addiction Inbox with the highest number of page views, an overwhelming majority are concerned with marijuana, and specifically, with marijuana addiction, withdrawal, and brain chemistry. Of the 9 most heavily trafficked posts of the year, only one involved alcohol. Readers were also interested in the safety of e-cigarettes, and the mysteries of neurotransmitters like serotonin and dopamine. Happily, all the top posts were patently science-oriented articles.
See you in the New Year.
For Some Users, Cannabis Can Be Fiercely Addictive.
For a minority of marijuana users, commonly estimated at 10 per cent, the use of pot can become uncontrollable, as with any other addictive drug. Addiction to marijuana is frequently submerged in the welter of polyaddictions common to active addicts. The withdrawal rigors of, say, alcohol or heroin tend to drown out the subtler, more psychological manifestations of cannabis withdrawal.
The Molecules of Reward
Serotonin and dopamine are part of a group of compounds called biogenic amines. In addition to serotonin and dopamine, the amines include noradrenaline, acetylcholine, and histamine. This class of chemical messengers is produced, in turn, from basic amino acids like tyrosine, tryptophan, and choline.
Why cannabis research is a good idea.
There is little doubt among responsible researchers that marijuana--although it is addictive for some people--is sometimes a clinically useful drug. However, there is little incentive for commercial pharmaceutical houses to pursue research on the cannabis plant itself, since they cannot patent it.
Anxiety and the THC receptor.
Several years ago, molecular biologists identified the elusive brain receptor where THC, the active ingredient in marijuana, did its work. Shortly after that discovery, researchers at Hebrew University in Jerusalem identified the body’s own form of THC, which sticks to the same receptors, in pulverized pig brains.
Why do so many smokers combine tobacco with marijuana?
People who smoke a combination of tobacco and marijuana, a common practice overseas for years, and increasingly popular here in the form of “blunts,” may be reacting to ResearchBlogging.orgsome unidentified mechanism that links the two drugs. Researchers believe such smokers would be well advised to consider giving up both drugs at once, rather than one at a time, according to an upcoming study in the journal Addiction.
A group of nicotine researchers argue for an alternative.
Electronic cigarettes are here to stay. If you're not familiar with them, e-cigarettes are designed to look exactly like conventional cigarettes, but they use batteries to convert liquid nicotine into a fine, heated mist that is absorbed by the lungs. Last summer, even though the FDA insisted on referring to e-cigarettes as “untested drug delivery systems,” Dr. Neal Benowitz of the University of California in San Francisco--a prominent nicotine researcher for many years--called e-cigarettes “an advancement that the field has been waiting for.”
Maybe it isn't endorphins after all.
A perennial favorite, the runner’s high post shows what long-distance running and marijuana smoking have in common. Quite possibly, more than you’d think. A growing body of research suggests that the runner’s high and the cannabis high are more similar than previously imagined….Endocannabinoids—the body’s internal cannabis—“seem to contribute to the motivational aspects of voluntary running in rodents.” Knockout mice lacking the cannabinioid CB1 receptor, it turns out, spend less time wheel running than normal mice.
Epilepsy drug gains ground, draws fire as newest anti-craving pill.
A drug for seizure disorders and migraines continues to show promise as an anti-craving drug for alcoholism, the third leading cause of death in America, the Journal of the American Medical Association (JAMA) reported in its current issue.
The argument continues.
Marijuana may not be a life-threatening drug, but is it an addictive one?
There is little evidence in animal models for tolerance and withdrawal, the classic determinants of addiction. For at least four decades, million of Americans have used marijuana without clear evidence of a withdrawal syndrome. Most recreational marijuana users find that too much pot in one day makes them lethargic and uncomfortable. Self-proclaimed marijuana addicts, on the other hand, report that pot energizes them, calms them down when they are nervous, or otherwise allows them to function normally.
Graphics Credit: http://1.bp.blogspot.com (Creative Commons)
Friday, October 19, 2012
Does Marijuana Withdrawal Matter?
What happens to some smokers when they cut out the cannabis.
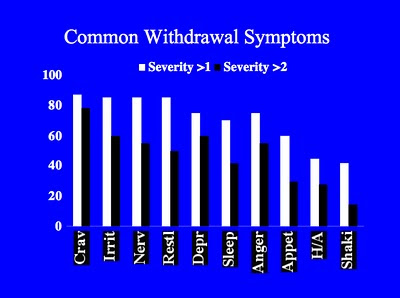
People who say they are addicted to marijuana tend to exhibit a characteristic withdrawal profile. But is cannabis withdrawal, if it actually exists, significant enough to merit clinical attention? Does it lead to relapse, or continued use despite adverse circumstances? Should it be added to the list of addictive disorders in the rewrite of the Diagnostic and Statistical Manual of Mental Disorders (DSM) currently in progress?
Marijuana fits in fairly well with the existing criteria for clinical addiction—except for one common diagnostic marker. Among the identifying criteria currently used in the DSM, we find: “The presence of characteristic withdrawal symptoms or use of substance to alleviate withdrawal.” Opponents of marijuana’s inclusion as an addictive drug have long insisted that cannabis has no characteristic withdrawal symptoms, but this position has been severely eroded of late, as new research has consistently identified a withdrawal syndrome for marijuana, which includes drug cravings, despite decades of controversy over this basic medical question.
A group of researchers at the University of New South Wales, Australia, along with Dr. Alan J. Budney of the Geisel School of Medicine at Dartmouth, New Hampshire, writing
(For more on the marijuana withdrawal profile, see HERE, and HERE. For a bibliography of relevant journal articles, go HERE).
But how does one go about determining if withdrawal reactions rise to the level of clinical significance? The researchers wanted to know whether functional impairment reported during abstinence was clinically significant, whether it correlated with severity of addiction, and whether it was predictive of relapse. 46 survey volunteers who were not seeking any formal treatment for marijuana addiction were recruited in Sydney, Australia. Users ranged in age from 18 to 57, with an average age of 30. After a one-week baseline phase, the participants underwent two weeks of monitored abstinence. Using a “Severity of Dependence Scale” (SDS) to measure variability in functional impairment, the researchers compared a high SDS subgroup to a low SDS subgroup in an effort to tease out whether functional impairments in high SDS participants were predictive of relapse. The researchers noted that earlier work had established that the symptoms most likely to cause impairment to normal daily functioning were: Trouble getting to sleep, angry outbursts, cravings, loss of appetite, feeling easily irritated, and nightmares or strange dreams.” The investigators broke these symptoms into two groups: “somatic” and “negative affect” variables.
The researchers then examined self-reports about the impact of cannabis withdrawal on normal daily activities. While the common yardstick for withdrawal is typically taken to be intensity of cravings, the authors argue that this reliance on craving “may mask the extent to which symptoms led to functional impairment, as those who maintained abstinence may still have experienced clinically significant negative consequences from cannabis withdrawal (e.g. relationship or work problems resulting from the withdrawal syndrome.”)
As might have been expected, higher levels of cannabis dependence were associated with greater functional impairment. And while the average level of functional impairment caused by cannabis is “mild for most users, it appears comparable with tobacco withdrawal which is of well established clinical significance.”
And certain symptoms were, in fact, correlative: “Increased somatic withdrawal symptoms are predictive of relapse, and…. increased physical tension is a significant predictor of relapse.”
Physical distress, a “somatic” variable, mattered more, in terms of relapse, than the amount of marijuana smoked, or any other symptom on the roster of functional impairments—including mood and other negative affect variables.
“In conclusion,” the investigators write, “cannabis withdrawal is clinically significant because it is associated with elevated functional impairment to normal daily activities, and the more severe the withdrawal is, the more severe the functional impairment is. Elevated functional impairment from a cluster of cannabis withdrawal symptoms is associated with relapse in more severely dependent users.”
Furthermore: “Targeting the withdrawal symptoms that contribute most to functional impairment during a quit attempt might be a useful treatment approach (e.g. stress management techniques to relieve physical tension and possible pharmacological interventions for alleviating the physical aspects of withdrawal such as loss of appetite and sleep dysregulation.)”
As with most studies, there are limitations. As noted, the participants were not in a formal cessation program. And while urine tests were used, there was no external corroboration of the self reports.
Allsop, D., Copeland, J., Norberg, M., Fu, S., Molnar, A., Lewis, J., & Budney, A. (2012). Quantifying the Clinical Significance of Cannabis Withdrawal PLoS ONE, 7 (9) DOI: 10.1371/journal.pone.0044864
Graphics Credit: http://www.addictionsearch.com/
Wednesday, August 15, 2012
Praising Marijuana Prohibition
As regular readers of Addiction Inbox will know, I am on record as favoring some form of decriminalization for marijuana. But I also write regularly about the difficulties of marijuana addiction and withdrawal. And I have been critical of the operational strategies employed by the medical marijuana movement in the several states in which it now operates. What I have not done, to date, is offer up the official view of a drug policy analyst from the Obama administration who straightforwardly favors a continuation of the legal prohibition against marijuana.
One of the architects of the current federal resistance to marijuana legalization is Kevin Sabet, an assistant professor and the director of the Drug Policy Institute at the University of Florida College of Medicine. Sabet served from 2009 to 2011 in the Obama Administration as Senior Advisor for the White House Office of National Drug Control Policy (ONDCP) under Drug Czar Gil Kerlikowske, and was influential in shaping federal marijuana policy. Sabet consults with governments and NGOs on a wide range of drug policy prevention issues, and recently debated legalization advocate Ethan Nadelmann on CNN. He is also a regular columnist for thefix.com and Huffington Post. He agreed to participate in a frank and lengthy 5-question interview with Addiction Inbox. (Be sure to check out the comments below).
1. In his new book, Too High to Fail, journalist Doug Fine argues that "the Drug War is as unconscionably wrong for America as segregation or DDT." Would you comment on this sweeping condemnation?
First, I think it is interesting to note that only people who want to condemn all of our current drug policies use the term "drug war." No one in serious policy circles uses that term anymore, and that is because it is woefully inadequate and vague as a way to describe a whole slew of policies designed to both reduce drug prevalence and drug consequences. I think his comparison is clumsy and unfair. Do some drug policies hurt disadvantaged groups? Of course they do. Is it a moral imperative to fix those policies, learn from our past mistakes and make our policies better? Of course it is. There's no reason to think that those policies can't be changed—in the White House in 2009, for example, we drastically reduced the penalty for crack cocaine. But what makes Mr. Fine's comparison even more wrong-headed and backwards is that we know that if we scale-up—not eliminate, as he would—the policies we know do work in reducing drug use and its consequences, all communities in America would benefit. A handful include:
(a) community-based prevention that not only focuses on stopping drug use among school kids, but in changing bad local laws and ordinances that promote underage drinking, smoking, and marijuana use (so-called "environmental policies");
(b) early intervention and detection of drug use in health settings;
(c) evidence-based treatment, including methadone and buprenorphine, as well as 12-step programs;
(d) recovery-based policies that don't penalize people for past drug use and instead facilitate recovery;
(e) law enforcement based on credible threats and modest sanctions.
2. The Drug War is an industry—the DEA alone has a budget of 2 1/2 billion and employs almost 10,000 people. If we add in profits from the private prison industry, and the money-laundering banks, the money is staggering. Wouldn't it make sense to recoup those historical costs by legalizing and taxing marijuana?
That phrase assumes two things: (a) criminal justice and regulation costs would be drastically reduced, or eliminated, with marijuana legalization; and (b) the underground market would be eliminated with marijuana legalization. Both of those assumptions are huge leaps that don't stand up to our experience with our already two legal drugs—alcohol and tobacco.
First, we know that legalization means more consumption. More consumption means more regulation. Today we have liquor laws, laws against drinking and driving, laws against public drunkenness, etc. With regards to legal alcohol, we make 2.6 million arrests every year for the violation of those laws. Meanwhile, we arrest a million fewer times for illegal drugs (1.6 million/year). Legal alcohol costs us money with regards to crime and regulation. I think that is a big consideration in this whole debate that we rarely hear about. So that means we'd have to have more prisons, more police, and more regulation costs under legalization—especially since few people are in prison or jail solely for marijuana use.
And I'm not so sure the underground market would be eliminated with marijuana legalization. Especially if it is taxed heavily, the incentive for the underground market—having been painstakingly established for decades by multinational corporate structures (cartels)—is very little. We'll still need a black market for underage marijuana, for marijuana to be sold to repeat offenders, etc. I just don't see the cartels throwing up their hands and saying "OK, it's legalized. We're out of the game now. Let's get into the ice cream business."
3. A "Pax Cannabis" would require rescheduling marijuana at the federal level, with an overt recognition that marijuana has some redeeming medical value. What's the argument for maintaining cannabis as a Schedule 1 drug along with heroin, a drug with which it has almost nothing in common? Could you comment on the upcoming U.S. Appeals Court consideration of medical marijuana?
Rescheduling marijuana is one of the biggest red herrings I can think of in this debate. If rescheduled tomorrow, it would do nothing to allow marijuana to be sold legally. Rather, it would be a huge symbolic victory for marijuana advocates -- but it would be wholly wrong on the science. Placing a drug in schedule 1 simply means the drug has no medical use and a high potential for abuse. It has nothing to do with the other drugs in that category (e.g. heroin). If it were a drug, a telephone would also need to be in Schedule 1 - I'm addicted to my cell phone and I know it has no medical use. That doesn't mean a phone is as dangerous as a syringe of heroin. Today, cocaine is Schedule 2 because it has some very limited hospital use. Can a 21-year-old kid with no medical knowledge sell cocaine from a "dispensary" called "Happy Clinic" legally? Of course not, though that is what is happening [with marijuana] in California.
In order to be used for medical use, a specific product needs to be approved by FDA. Marijuana's specific product, so far, is Marinol, a Schedule 3 drug which has been approved by FDA and is used by people throughout the world. Crude, raw marijuana is not a specific product. The best way I can put it is this: We don't smoke opium to get the effects of morphine, so why do we think we need to smoke marijuana to get its potential medical effects? We have non-inhaled medications that are approved and we have others on the way. For a lot more on this, you can check out an article I wrote for Join Together. I think the District court opinion will rest on the science and agree with the Department of Health and Human Services that raw, crude marijuana is not medicine.
4. Alaska decriminalized marijuana in 1975, and only recriminalized after lengthy pressure from the Reagan administration. Isn't cultivation of this flowering weed for personal use the most obvious and straightforward solution?
The Reagan Administration could have cared less about Alaska, frankly. Alaska recriminalized because voters there wanted that to happen. They didn't like the effect of decriminalization on their state. That said, I don't think many people are in favor—and I am not—of locking up people smoking small amounts of marijuana. That isn't happening anywhere. One notable exception is New York City where they impose 24-hour detentions for public use and selling as part of their broken windows approach to crime control.
Indeed, in the 1970s, twelve states formally decriminalized marijuana. This meant that persons found to have a small amount of marijuana were not subject to jail time, but rather they would receive a civil penalty, such as a fine. The discussion in the United States is highly complex because even in jurisdictions without a formal decriminalization law, persons are rarely jailed for possessing small amounts of cannabis. A rigorous government analyses of who is in jail or prison for marijuana found that less than 0.7% of all state inmates were behind bars for marijuana possession only (with many of them pleading down from more serious crimes).[1] Other independent research has shown that the risk of arrest for each “joint,” or cannabis cigarette, smoked is about 1 arrest for every 12,000 joints.[2] This probably explains the fact that the literature on early decriminalization effects on use has been mixed. Some studies found no increase in use in the so-called “depenalization” states, whereas others found a positive relationship between greater use and formal changes in the law.[3]
The more recent discussion about state-level legalization may provide more insights. Two RAND Corporation reports concluded that legalization would result in lower cannabis prices, and thus increases in use (though by how much is highly uncertain), and that “legalizing cannabis in California would not dramatically reduce the drug revenues collected by Mexican drug trafficking organizations from sales to the United States.”[4]
5. Marijuana advocates don't like to hear it, but pot is addictive for some users. Where do you stand on this controversial issue?
Science tells us that marijuana is addictive—about 1 in 11 people who ever smoke marijuana are addicted; but if you start in adolescence that number climbs to 1 in 6. That's not anyone's opinion but rather the result of rigorous scientific research done by the National Institutes of Health and confirmed by other international scientific bodies. Is marijuana as addictive as tobacco cigarettes? No. The addiction rate for tobacco is about 1 in 3; for heroin it is lower, about 1 in 4. Users who try to quit experience withdrawal symptoms that include irritability, anxiety, insomnia, appetite disturbance, and depression.
A United States study that dissected the National Longitudinal Alcohol Epidemiologic Survey (conducted from 1991 to 1992 with 42,862 participants) and the National Epidemiologic Survey on Alcohol and Related Conditions (conducted from 2001 through 2002 with more than 43,000 participants) found that the number of cannabis users stayed the same while the number dependent on the drug rose 20 percent from 2.2 million to 3 million.[5]Authors speculated that higher potency marijuana may have been to blame for this increase. As I've heard said many times by experienced tokers, "this isn't your Grandfather's Woodstock Weed."
[1] “Substance Abuse and Treatment, State and Federal Prisoners, 1997.” BJS Special Report, January 1999, NCJ 172871. http://www.ojp.usdoj.gov/bjs/pub/pdf/satsfp97.pdf
[2] Beau Kilmer, Jonathan P. Caulkins, Rosalie Liccardo Pacula, Robert J. MacCoun, Peter H. Reuter, Altered State? Assessing How Cannabis Legalization in California Could Influence Cannabis Consumption and Public Budgets, RAND, 2010.
[3] For a discussion see MacCoun, R., Pacula, R. L., Reuter, P., Chriqui, J., Harris, K. (2009). Do citizens know whether they live in a decriminalization state? State cannabis laws and perceptions. Review of Law & Economics, 5(1), 347-371.
[4] Beau Kilmer, Jonathan P. Caulkins, Rosalie Liccardo Pacula, Robert J. MacCoun, Peter H. Reuter, Altered State? Assessing How Cannabis Legalization in California Could Influence Cannabis Consumption and Public Budgets, RAND, 2010. And see Kilmer, Beau , Jonathan P. Caulkins, Brittany M. Bond and Peter H. Reuter. Reducing Drug Trafficking Revenues and Violence in Mexico: Would Legalizing Cannabis in California Help?.Santa Monica, CA: RAND Corporation, 2010. http://www.rand.org/pubs/occasional_papers/OP325. Also available in print form.
[5] ]Compton, W., Grant, B., Colliver, J., Glantz, M., Stinson, F. Prevalence of Cannabis Use Disorders in the United States: 1991-1992 and 2001-2002Journal of the American Medical Association.. 291:2114-2121.
Photo Credit:http://article.wn.com/
Tuesday, April 24, 2012
A Drug For Marijuana Withdrawal?
Researchers get good results with gabapentin.
Marijuana, as researchers and pundits never tire of pointing out, is the most widely used illegal drug in the world, by a serious margin. And while the argument still rages, for some years now drug researchers have been migrating to the camp that sees marijuana as an addictive drug for a minority of people who exhibit a propensity for addiction. The scientific literature supporting the contention of marijuana as addictive for some users is robust and growing, as is the body of anecdotal evidence. It’s also clear that in many countries, cultures, and subcultures, combining cannabis with tobacco is a common practice that increases health risks all around.
Ongoing work at the Scripps Research Institute’s Pearson Center for Alcoholism and Addiction Research in La Jolla, California, has focused in part on the lack of FDA-approved medical therapies for treating marijuana addiction. Barbara J. Mason and
Marijuana addiction numbers are hard to come by, and often inflated, since many small-time pot offenders end up in mandatory treatment programs, where they tend to be classified as marijuana addicts, whether or not that is objectively the case. Nonetheless, there are plenty of people seeking treatment on their own for cannabis dependence. For people strongly addicted to pot, the problems are very real, and withdrawal and abstinence pose serious challenges. People for whom marijuana poses no addictive threat should bear this in mind, the way casual drinkers bear in mind the existence of alcoholism in others.
The study, published recently in Neuropsychopharmacology, says that “activation of brain stress circuitry caused by chronic heavy marijuana use” can lead to withdrawal symptoms that persist “for weeks or even months, as in the case of marijuana craving and sleep disturbances.” A variety of existing medications have been tested in recent years, including buspirone, an anti-anxiety medication; Serzone, an antidepressant; and Wellbutrin, an antidepressant commonly used for smoking cessation. None of these treatments has shown any effect on cannabis use or withdrawal, according to Mason.
Gabapentin, as the name suggests, was modeled after the neurotransmitter GABA, and works via a transporter protein to raise GABA levels. Effective only for partial-onset seizures, common side effects include drowsiness, dizziness, and possible weight gain. It is a popular anti-epileptic drug, because it is relatively safe, with a low side-effect profile, compared to many of the medications in its class. For the same reasons, it is a common treatment for neuropathic pain. In addition to neuralgia, it has found some use as a migraine preventative.
Gabapentin normalizes GABA activation caused by corticotrophin-releasing factor, or CRF. CRF is a major player in the brain’s stress responses. As it turns out, withdrawal from both cannabis and alcohol ramp up anxiety levels by increasing CRF release in the amygdala, animal studies have shown. “Gabapentin had a significant effect in decreasing marijuana use over the course of treatment, relative to placebo,” the authors report. In addition, gabapentin produced “significant reductions in both the acute symptoms of withdrawal as well as in the more commonly persistent symptoms involving mood, craving, and sleep.”
As a bonus, the researchers discovered that “overall improvement in performance across cognitive measures was significantly greater for gabapentin-treated subjects compared with those receiving placebo.” Gabapentin was associated with improvement in “tasks related to neurocognitive executive functioning”—things like attention, concentration, visual-motor functioning, and inhibition. Counseling alone, represented by the placebo group, “resulted in less effective treatment of cannabis use and withdrawal, and no improvement in executive function.”
As in the case of Chantix for cigarette cessation, a treatment, which now requires additional caveats about possible suicidal ideation, researchers looking for a treatment for drug withdrawal, must weigh the benefits of pharmacological treatment against the possible side effects of the treatment itself. Does gabapentin for marijuana withdrawal pass the “Do No Harm” test? According to Mason, it does. “Gabapentin was well tolerated and without significant side effects” in the admittedly small trial study. The two groups did not differ in the number of adverse medical events reported in the first two weeks, when dropout rates due to side effects are highest in these kinds of studies. The investigators were not relying solely on self-reporting, either. They used urine drug screens, and verified that only 3% of the study sample tested positive for other drugs.
In short, the authors report that gabapentin reduced cannabis use and eased withdrawal with an acceptable safety profile and no signs of dependence. Gabapentin, the authors conclude, “may offer the most promising treatment for cannabis withdrawal and dependence studied to date.” Further clinical research is needed, of course, but the positive results of this proof-of-concept study should make funding a bit easier.
Mason, B., Crean, R., Goodell, V., Light, J., Quello, S., Shadan, F., Buffkins, K., Kyle, M., Adusumalli, M., Begovic, A., & Rao, S. (2012). A Proof-of-Concept Randomized Controlled Study of Gabapentin: Effects on Cannabis Use, Withdrawal and Executive Function Deficits in Cannabis-Dependent Adults Neuropsychopharmacology DOI: 10.1038/npp.2012.14
Photo Credit: http://pep3799.hubpages.com/
Thursday, March 22, 2012
The Mysteries of the Blunt
Why do so many smokers combine tobacco with marijuana?
People who smoke a combination of tobacco and marijuana, a common practice overseas for years, and increasingly popular here in the form of “blunts,” may be reacting to
Clinical trials of adults with cannabis use disorders suggest that “approximately 50% are current tobacco smokers,” according to the report, which was authored by Arpana Agrawal and Michael T. Lynskey of Washington University School of Medicine, and Alan J. Budney of the University of Arkansas for Medical Sciences. “As many cannabis users smoke a mixture of cannabis and tobacco or chase cannabis use with tobacco, and as conditioned cues associated with smoking both substances may trigger use of either substance,” the researchers conclude, “a simultaneous cessation approach with cannabis and tobacco may be most beneficial.”
A blunt is simply a marijuana cigar, with the wrapping paper made of tobacco and the majority of loose tobacco removed and replaced with marijuana. In Europe, smokers commonly mix the two substances together and roll the combination into a single joint, the precise ratio of cannabis and nicotine varying with the desires of the user. “There is accumulating evidence that some mechanisms linking cannabis and tobacco use are distinct from those contributing to co-occurring use of drugs in general,” the investigators say. Or, as psychiatry postdoc Erica Peters of Yale put it in a press release, “There’s something about tobacco use that seems to worsen marijuana use in some way.” The researchers believe that this “something” involved may be a genetic predisposition. In addition to an overall genetic proclivity for addiction, do dual smokers inherit a specific propensity for smoked substances? We don’t know—but evidence is weak and contradictory so far.
Wouldn’t it be easier to quit just one drug, using the other as a crutch? The researchers don’t think so, and here’s why: In the few studies available, for every dually addicted participant who reported greater aggression, anger, and irritability with simultaneous cessation, “comparable numbers of participants rated withdrawal associated with dual abstinence as less severe than withdrawal from either drug alone.” So, for dual abusers, some of them may have better luck if they quit marijuana and cigarettes at the same time. The authors suggest that “absence of smoking cues when abstaining from both substances may reduce withdrawal severity in some individuals.” In other words, revisiting the route of administration, a.k.a. smoking, may trigger cravings for the drug you’re trying to quit. This form of “respiratory adaption” may work in other ways. For instance, the authors note that, “in addition to flavorants, cigarettes typically contain compounds (e.g. salicylates) that have anti-inflammatory and anesthetic effects which may facilitate cannabis inhalation.”
Studies of teens diagnosed with cannabis use disorder have shown that continued tobacco used is associated with a poor cannabis abstention rate. But there are fewer studies suggesting the reverse—that cigarette smokers fair poorly in quitting if they persist in cannabis use. No one really knows, and dual users will have to find out for themselves which categories seems to best suit them when it comes time to deal with quitting.
We will pass up the opportunity to examine the genetic research in detail. Suffice to say that while marijuana addiction probably has a genetic component like other addictions, genetic studies have not identified any gene variants as strong candidates thus far. The case is stronger for cigarettes, but to date no genetic mechanisms have been uncovered that definitively show a neurobiological pathway that directly connects the two addictions.
There are all sorts of environmental factors too, of course. Peer influences are often cited, but those influences often seem tautological: Drug-using teens are members of the drug-using teens group. Tobacco users report earlier opportunities to use cannabis, which might have an effect, if anybody knew how and why it happens.
Further complicating matters is the fact that withdrawal from nicotine and withdrawal from marijuana share a number of similarities. The researchers state that “similar withdrawal syndromes, with many symptoms in common, may have important treatment implications.” As the authors sum it up, cannabis withdrawal consists of “anger, aggression or irritability, nervousness or anxiety, sleep difficulties, decreased appetite or weight loss, psychomotor agitation or restlessness, depressed mood, and less commonly, physical symptoms such as stomach pain and shakes/tremors.” Others complain of night sweats and temperature sensitivity.
And the symptoms of nicotine withdrawal? In essence, the same. The difference, say the authors, is that cannabis withdrawal tends to produce more irritability and decreased appetite, while tobacco withdrawal brings on an appetite increase and more immediate, sustained craving. Otherwise, the similarities far outnumber the differences.
None of this, however, has been reflected in the structure of treatment programs: “Emerging evidence suggests that dual abstinence may predict better cessation outcomes, yet empirically researched treatments tailored for co-occurring use are lacking.”
The truth is, we don’t really know for certain why many smokers prefer to consume tobacco and marijuana in combination. But we do know several reasons why it’s not a good idea. Many of the health-related harms are similar, and presumably cumulative: chronic bronchitis, wheezing, morning sputum, coughing—smokers know the drill. Another study cited by the authors found that dual smokers reported smoking as many cigarettes as those who only smoked tobacco. All of this can lead to “considerable elevation in odds of respiratory distress indicators and reduced lung functioning in those who used both.” However, there is no strong link at present between marijuana smoking and lung cancer.
Some researchers believe that receptor cross-talk allows cannabis to modify receptors for nicotine, or vice versa. Genes involved in drug metabolism might somehow predispose a subset of addicts to prefer smoking. But at present, there are no solid genetic or environmental influences consistent enough to account for a specific linkage between marijuana addiction and nicotine addiction, or a specific genetic proclivity for smoking as a means of drug administration.
Agrawal, A., Budney, A., & Lynskey, M. (2012). The Co-occurring Use and Misuse of Cannabis and Tobacco: A Review Addiction DOI: 10.1111/j.1360-0443.2012.03837.x
Photo credit: http://stuffstonerslike.com
Thursday, April 7, 2011
Marijuana, Vomiting, and Hot Baths
A case history of cannabinoid hyperemesis.
Cannabinoid hyperemesis, as it's known, is an extremely rare but terrifying disorder marked by severe episodic vomiting that can only be relieved by hot baths. (see earlier post). Sufferers are heavy, regular cannabis users, most of them. And hot baths? Where did THAT come from?
The syndrome was first brought to wider attention last year by the anonymous biomedical researcher who calls himself Drugmonkey, who documented cases of hyperemesis that had been reported in Australia and New Zealand, as well as Omaha and Boston in the U.S. "There were two striking similarities across all these cases," Drugmonkey reported. "The first is that patients had discovered on their own that taking a hot bath or shower alleviated their symptoms. So afflicted individuals were taking multiple hot showers or baths per day to obtain symptom relief. The second similarity is, as you will have guessed, they were all cannabis users."
The reports haven't stopped. This summer, an intriguing account appeared on the official blog of New York University's Division of General Internal Medicine, where med students offered a formal definition: "A clinical syndrome characterized by intractable vomiting and abdominal pain associated with the unusual learned behavior of compulsive hot water bathing, occurring in the setting of long-term heavy marijuana use."
Still skeptical? I received this heartfelt comment on my original post a few days ago:
Listen, doubters. My son has this. He has been cyclical vomiting and spending hours in boiling hot baths since last Autumn. It's getting worse and he has lost a hell of a lot of weight. He is 21 and an addicted, heavy cannabis user who started at 15. He has tried cutting down but every other joint of weed brings on the obsession. He refuses to co operate with medical staff who try to treat him.
He has been taken to numerous hospitals as an emergency for non-stop vomiting and begs medical staff to let him sit in a very hot bath. They try the best anti-vomiting drugs instead, to no effect, and then some let him go in a hot shower for an hour plus. He always ends up on a drip and as soon as he feels well enough, discharges himself, often the same day.
At the weekend he went to a sports event in the city with friends, realised on the way he was going to have an episode, so left friends and made his way into a hotel room and locked himself in. Police were called and got him out of a boiling hot bath against his will. Cue vomiting attack so bad police called an ambulance. Once again discharged himself from hospital, demanding drip be removed or he would do it himself. Has sat in bath at house he shares with girlfriend for at least 12 hours today, she tells me. She says water is so hot she has no idea how he bears it.
He says he has no pain in stomach, just a sensation that drives his head mad and he KNOWS it will not go, or the vomiting stop, until he gets in boiling hot bath and stays there. He has even done this while abroad on holiday and ended up on a drip before being flown home.
All of this is true. A mother.
I was intrigued, and discussed this briefly with the mother, who lives in the U.K. She added a number of details in an email exchange, and agreed to let me publish her comments:
“I am a mother in the UK whose son definitely has this, but is not officially diagnosed as he ‘escapes’ medical attention by discharging himself from various hospitals.
When it happens he is desperate to get in a hot bath. He lives with his girlfriend. I only realised what the hell was really going on when she insisted on telling me, and have since been regularly involved in the hospitals saga.
When I discovered the truth I put ‘cannabis’ ‘vomiting’ and ‘hot baths’ ‘showers’ in google and up came a perfect description of what my son does.
I am trying to get him to agree to go for counselling and psychiatric help as he has reached the stage where this obsessive vomiting and bathing is wrecking his life. But every time he gets a little better he believes he can ‘control it’ which is not the case at all.
Yes – we end up in the hospitals and the first young emergency doctor who has ever smoked a joint and/or thinks he knows everything, tells G “Oh no it can’t be that, cannabis stops vomiting, not starts it.” Of course, they have never heard of this condition and just think he is being irrational because of the constant need to vomit. They are sure it is food poisoning or some kind of spasm and take basic blood tests.
They find nothing, insist on giving him the best anti-sickness drugs usually for cancer patients and so on…, saying “this will definitely stop it” and still he vomits. He is not in pain, just rapidly dehydrating and panicking and complaining of a weird sensation in his stomach. He tells them “I know it’s in my head doing this” and desperately demands to get in a bath. Even when he has arrived at hospital because police found him in a boiling hot bath, this makes no sense to the medics who only give in when none of their drugs work. He then immediately stops vomiting but is petrified of getting out of the bath. Eventually, when he says it is under control, he agrees to get out, and is put on a drip. Approx an hour later, while the doctors are planning follow-up procedures like scans and more complex blood tests etc, he starts an argument with a nurse, insists the drip is removed and phones a friend to collect him, avoiding seeking a lift from me if he can. The over-pressed doctors here (the British system is like a cattle market) are left mystified and move onto the next emergency in their pile up of admissions. And so it goes on, and will do, until G accepts even the odd joint can set him off.”
----
Researchers speculate that it has something to do with CB-1 cannabinoid receptors in the intestinal nerve plexus--but nobody really knows for sure. Low doses of THC might be anti-emetic, whereas in certain people, the high concentrations produced by long-term use could have the opposite effect.
Monday, March 7, 2011
Seeking a Patch or a Pill for Pot
Drug treatments for marijuana withdrawal.
Sometimes it’s easy to forget that marijuana is the most widely used illegal drug of all. We demonize it, yet we take it for granted. We punish citizens for its possession, but we call it a “soft” drug.
The idea of marijuana as an addictive drug--for some but by no means all users—still seems preposterous to a large number of recreational pot smokers. Yet these same people have far less trouble dealing with the existence of raging alcoholics surrounded by a majority of controlled, recreational drinkers or non-drinkers.
For purposes of this post, we are going to stipulate that sufficient scientific evidence now exists to include marijuana in the category of addictive psychoactive drugs. Heavy, daily users of marijuana sometimes find themselves in an unexpected bind if they decide to quit cold. Perhaps as many as one or two in every ten heavy pot smokers will find themselves suffering from flu-like symptoms, loss of appetite, insomnia, vivid dreams, irritability, generalized anxiety, and other side effects that can be at least as unpleasant as quitting cold turkey after a long cigarette habit.
Why didn’t we know this earlier? Perhaps for the same reasons that we didn’t know until the 1980s, as a general piece of knowledge, that cocaine was highly addictive. (Marijuana Anonymous didn’t start up until 1989). Doesn’t that sound absurd now, the state of our understanding of cocaine’s effects only 30 years ago? For people who suffer strong and repeatable withdrawal symptoms when they try to quit smoking weed, it is equally absurd to proclaim that what they are wrestling with does not resemble a genuine drug addiction (See the Addiction Inbox thread on marijuana withdrawal, which is now approaching 1,000 comments, and which constitutes a major database of self-reported data on marijuana withdrawal).
Having identified marijuana as classically addictive for a small slice of the user population, the focus has lately turned toward human laboratory studies, although most of the human studies thus far have been open-label trials rather than controlled double-blind studies. A group of researchers at Columbia University has been testing a variety of medications in search of a compound with demonstrated effects on marijuana abstinence and withdrawal. A study published online last year examines the effectiveness of a variety of medications on the course of marijuana craving and withdrawal in users classified as marijuana dependent. In other words, they are looking for the equivalent of a nicotine patch for marijuana.
Nonetheless, the marijuana withdrawal syndrome is now well established in the scientific literature, as well as anecdotally. Among heavy dope smokers, the authors write, cold-turkey cessation from marijuana “produces cellular changes in the brain reward pathway (increased corticotrophin-releasing factor, decreased dopamine) that have been linked to the dysphoric effects associated with withdrawal from drugs such as alcohol, opiates, and cocaine, and are thought to contribute to relapse.”
What have they discovered so far?
One obvious starting point was dronabinol, a.k.a. Marinol, the government-approved synthetic THC often prescribed for nausea, vomiting, and appetite loss due to chemotherapy. Marinol is a direct approach to the nicotine patch strategy: A substance that stimulates cannabis receptors in a manner similar to, but by no means identical with, the high produced by natural marijuana. Perhaps a regular low dose of Marinol would keep the cannabis cravings at bay among problem users trying to quit. As it turns out, not really. Some studies showed that you could reduce a pot addict’s withdrawal symptoms somewhat in a home environment with Marinol, but the dose required to accomplish this was high enough to represent potential problems of its own.
Another obvious candidate for investigation was rimonabant, a.k.a. Accomplia—but for the opposite reason. Rimonabant, which started out life as an anti-obesity medication, blocks the cannabinoid receptor CB1, so in that sense it should function roughly like Antabuse for alcoholics. It is the “anti-weed,” but as it turned out, rimonabant’s effect on cannabis receptors didn’t do the trick, either. Rimonabant “reduced the effects of smoked cannabis in two studies,” Vandrey and Haney write, “but a reduction of subjective drug effects was not consistently observed.” Furthermore, rimonabant is under suspicion for causing “adverse psychiatric effects” and is not much in favor at present.
Next up, naltrexone—an opiod receptor antagonist, which blocks the effects of heroin and is used in alcohol and heroin detox and withdrawal. Naltrexone has been shown in some studies to “reduce the subjective effects of cannabinoids in humans,” the authors note. But no dice: “In cannabis users, pretreatment with high doses of naltrexone (50-200 mg) failed to attenuate, and in some cases enhanced, the subjective effects of dronabinol and smoked cannabis.” To make matters worse, “the effect of naltrexone can be overcome with higher doses of cannabis.”
Other possible anti-craving drugs for marijuana have not been as rigorously studied. An open-label investigation of buspirone, which works on serotonin and dopamine systems, caused a decline in self-reported cannabis use, and pot smokers showed marked decreases in craving and irritability—but, as these things often go, buspirone was not well-tolerated by the participants, with too many dropouts due to adverse side effects.
Lithium, a mood stabilizer commonly prescribed for bipolar disorder, has shown promise in several small studies. An open-label lithium trial by the National Drug and Alcohol Research Centre in New South Wales resulted in “significant reductions in symptoms of depression and anxiety and cannabis-related problems.” More studies are needed.
Fluoxetine, better known to the world as Prozac, has been anecdotally associated with reduced marijuana use in depressed alcohol-dependent patients, but has never been the subject of any large clinical studies with a population of users whose primary drug is marijuana.
And finally, there is a dark-horse candidate, a treatment drug sometimes employed to prevent relapse
in cases of heroin addiction. Lofexidine is an alpha-2-adrenergic agonist that has been in use for years in the U.K. under the name BritLofex to treat the common symptoms of heroin withdrawal, such as cramps, chills, sweating, loss of appetite, and diarrhea. Similar but less intense withdrawal symptoms also afflict heavily addicted marijuana users. In a 2008 paper published in Psychopharmacology, “lofexidene was sedating, worsened abstinence-related anorexia, and did not robustly attenuate withdrawal, but improved sleep and decreased marijuana relapse.” Lofexidine combined with THC yielded even better results.
It appears that immediate research might be most profitably focused on lofexidine and lithium. And indeed, additional studies of the two drugs for cannabis dependency are planned by NIDA. Also, the combination of dronabinol and lofexidine appears to be worth pursuing in future clinical investigations of anti-craving drugs for marijuana.
Vandrey, R., & Haney, M. (2009). Pharmacotherapy for Cannabis Dependence CNS Drugs, 23 (7), 543-553 DOI: 10.2165/00023210-200923070-00001
Graphics Credit: http://archives.drugabuse.gov
Wednesday, April 14, 2010
Detoxifying with Marijuana Anonymous
What MA has to say.
Marijuana Anonymous was formed in 1989 as a program for those having difficulty remaining abstinent from marijuana. It is based on the 12-Step approach formulated by Alcoholics Anonymous. The group was founded in California as an amalgamation of existing groups, such as Marijuana Smokers Anonymous in southern California and Marijuana Addicts Anonymous in San Francisco. (In 1978, Pot Smokers Anonymous was founded in New York by David and Pearl Izenzon.)
But what, exactly, does Marijuana Anonymous say about marijuana? What does the organization actually suggest, in addition to the 12 Steps, when it comes to abstaining from cannabis?
The following information was excerpted from the official home page of Marijuana Anonymous and from pamphlets made available by the group.
Can there be physical effects from quitting marijuana?
In spite of numerous years of being told that there are no physiological effects from marijuana addiction, many of our recovering members have had definite withdrawal symptoms. Whether the causes are physical or psychological, the results are physical. Others have just had emotional and mental changes as they stop using their drug of choice. There is no way of telling before quitting who will be physically uncomfortable and who will not. Most members have only minor physical discomfort if any at all. This pamphlet is for those who are having trouble and wonder what's happening to them.
What are some of the more common symptoms?
By far the most common symptom of withdrawal is insomnia. This can last from a few nights of practically no sleep at all, up to a few months of occasional sleeplessness. The next most common symptom is depression (that is, if you're not euphoric), and next are nightmares and vivid dreams. Marijuana use tends to dampen the dreaming mechanism, so that when you do get clean the dreams come back with a crash. They can be vivid color, highly emotional dreams or nightmares, even waking up then coming back to the same dream. The very vivid, every-night dreams usually don't start for about a week or so.
The fourth most common symptom is anger. This can range from a slow burning rage to constant irritability to sudden bursts of anger when least expected: anger at the world, anger at loved ones, anger at oneself, anger at being an addict and having to get clean. Emotional jags are very common, with emotions bouncing back and forth between depression, anger, and euphoria. Occasionally experienced is a feeling of fear or anxiety, a loss of the sense of humor, decreased sex drive, or increased sex drive. Most all of these symptoms fade to normal emotions by three months. Loss of concentration for the first week or month is also very common and this sometimes affects the ability to learn for a very short while.
What about physical symptoms?
The most common physical symptom is headaches. For those who have them, they can last for a few weeks up to a couple of months, with the first few days being very intense. The next most common physical symptom is night sweats, sometimes to the point of having to change night clothes. They can last from a few nights to a month or so.
One third of the addicts who responded to a questionnaire on detoxing said they had eating problems for the first few days and some for up to six weeks. Their main symptoms were loss of appetite, sometimes enough to lose weight temporarily, digestion problems or cramps after eating, and nausea, occasionally enough to vomit (only for a day or two). Most of the eating problems were totally gone before the end of a month.
The next most common physical symptoms experienced were tremors or shaking and dizziness. Less frequently experienced were kidney pains, impotency, hormone changes or imbalances, low immunity or chronic fatigue, and some minor eye problems that resolved at around two months.
For more information, contact:
Marijuana Anonymous World Services
P.O. Box 2912
Van Nuys, CA 91404
USA
Toll Free 1-800-766-6779
office@marijuana-anonymous.org
graphic: http://www.7h1s.com/ ©2008 - Marijuana Anonymous World Services - All Rights Reserved.
Tuesday, March 16, 2010
Marijuana Q & A
Denny Chapin, Managing Editor of AllTreatment.com, was recently invited to participate in an extended debate over marijuana withdrawal at the Drug WarRant blog site. I followed that debate with interest, due to the unusually high volume of responses to my own post on that subject.
Now Denny has kindly provided me the opportunity to offer my own views on a set of questions about cannabis use and cannabis dependency. The complete interview can be read at the AllTreatment site HERE.
Photo credit: http://www.medicalmarijuana.co.cc
Wednesday, January 13, 2010
The Addiction Inbox Top Ten
What are readers of Addiction Inbox interested in? Although scarcely scientific, a look at the most-viewed posts here over the past couple of years is indicative of general interest—or at least indicative of the general drift of Google searches on topics related to addiction and drugs.
Ranked by overall page views, from most to least, here are the ten most-visited blog posts on Addiction Inbox:
The most popular post on Addicton Inbox by a considerable margin. With almost 700 reader comments, this post has evolved into a message board for people having problems related to marijuana dependence and withdrawal. Very interesting first-person stuff attached to a rather straightforward post. Continues to grow like Topsy.
A continuation of the discussion of marijuana withdrawal, or, as the director of the National Institute on Drug Abuse (NIDA) Nora Volkow calls it, “cannabis withdrawal syndrome.” 100 reader comments thus far.
Sometimes you just gotta get back to basics. Inquiring readers want to know.
A lively debate on the new, smokeless nicotine delivery system. Electronic cigarettes use batteries to convert liquid nicotine into a heated mist that is absorbed by the lungs. The latest in harm reduction strategies, or starter kits for youngsters?
Another good response to a medical post about a drug for seizure disorders and migraines that shows promise as an anti-craving drug for alcoholism. People are getting more accustomed to hearing about medications for addiction.
Not a big surprise.
Another comment-heavy post concerning a controversial study of withdrawal effects from smoking cigarettes and pot.
Something of a merger here between two consistently popular topics--cannabis and brain science. After the Sanskrit “ananda,” meaning bliss.
Readers seem to take seriously the notion that certain forms of overeating are substance addictions. This post focused on sugar's drug-like effect on the nucleus accumbens, a dopamine-rich brain structure in the limbic system.
10. Coffee Addiction
Increased tolerance, craving, and verifiable withdrawal symptoms--the primary determinants of addiction--are easily demonstrated in victims of caffeinism.
Subscribe to:
Posts (Atom)